Psychiatry
Medicine’s Way of Thinking Prevents Progress in Psychiatry
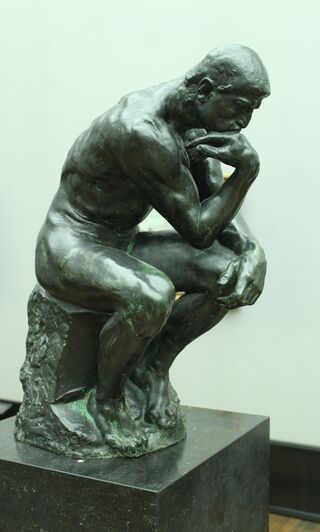
“Looking where the light is.”
Posted May 28, 2020
In a previous post, you heard how Rene Descartes and other Enlightenment philosophers split the mind and its mental operations from the body, leaving medicine with an almost exclusive focus on the physical body and its diseases. Beneficial as this was to modern medicine, an unintended consequence was leaving mental health issues behind. Evidence for this is the failure to train primary care and other medical physicians in mental health care even though they provide 85% of it.
In another post, I reviewed that, if modern medicine is to progress, it must adopt the same systems thinking other sciences have already deployed. In medicine, a systems approach takes the form of the biopsychosocial (BPS) model. It integrates the now missing psychological (mental) and social dimensions of patients with the biomedical (disease) component.
In this post, I will discuss how medicine’s thinking precludes expansion to the BPS model.1 While some in medicine recognize the mental health problem, the thought process needed to effectively incorporate it is thwarted by the profession’s inability to think outside the constraints of its Cartesian heritage.
Watzlawick calls this “level confusion,” meaning medicine is trying to solve the mental health problem at one conceptual level (psychological and social) using thinking that applies to a different level (disease).1 Solving refractory problems almost always involves thinking at a new level, second order thinking rather than, in medicine, first order thinking restricted to diseases.1,2 Medicine has a long history of painfully ineffective first order efforts to correct the mental health problem, for example, providing better insurance payments for mental health care by (untrained) primary care physicians, reducing competing demands on (untrained) physicians to give them more time for patients with mental problems, and providing (seldom available) psychiatric consultation to the (untrained) physician. (While the latter is effective,3 implementation over the last 20 years has been difficult because of the extreme shortage of psychiatrists.4)
Because first order thinking has been effective for problems at the disease level, second order thinking appears illogical to much of medicine. Making change still more problematic, first order thinking became deeply ingrained because medicine succeeded famously with acute diseases (such as strep throat, pneumonia, or appendicitis). Psychosocial issues were less important than, for example, antibiotics and surgery. But, as patients now lived longer, success spawned failure.
The unexpected result of its success with acute diseases was that mental health problems and chronic diseases replaced acute diseases as the predominant health care issue. Discussed in another post, psychosocial factors emerged as the key not only in mental disorders but also in chronic diseases where mental disorders and other psychosocial factors are prime determinants of disease outcomes.
Yet, medicine continues to think in terms of diseases, paying only token attention to psychosocial issues. Has its thinking arrested, seduced by its successes with acute diseases to think all problems can be solved this way? We see evidence of this in its efforts to find a disease explanation for mental disorders, for example, in its narrow focus on medications and the belief that the genome project will provide all the answers.
How do we solve this? From a BPS perspective, medicine’s thinking process must expand beyond physical diseases to integrate an equal focus on the psychological and social determinants of mental health, for example, the stress of difficult personal relationships, job loss, poverty, and abuse. These patients develop depression and anxiety but usually do not have a disease causing it. There are indeed some problems where a disease/genetic problem, such as schizophrenia, causes mental illness, but more often there is no physical basis. It’s the psychological and social factors that have to be addressed primarily—exactly what medicine’s present conceptual approach eschews.
This may remind you of the old story of a man looking for a lost object “where the light is” rather than where the problem is, that is, doing what you know rather than addressing the new, different problem.1 Only by thinking out of the box can medicine get to the BPS model and overcome a century of failure in mental health care where, according to Thomas Insel, we are no closer to a solution than we were 25 years ago.5
How will we know when medicine wakens? As I proposed in my initial post, they will train the physicians who provide mental health and other psychosocial care. Right now they receive little or no training for the most common problems they encounter in practice. Using second order thinking, medicine could solve this problem tomorrow.
References
1. Watzlawick P, Weakland JH, Fisch R. Change: Principles of Problem Formation and Problem Resolution. New York: WW Norton & Company, Inc.; 1974.
2. Ambrose D. Large-Scale Interdisciplinary Design Thinking for Dealing with Twenty-First Century Problems and Opportunities. In: Darbellay F, Moody Z, Lubart T, eds. Creativity, Design Thinking and Interdisciplinarity. New York: Springer; 2017:35-52.
3. Huffman JC, Niazi SK, Rundell JR, Sharpe M, Katon WJ. Essential Articles on Collaborative Care Models for the Treatment of Psychiatric Disorders in Medical Settings: A Publication by the Academy of Psychosomatic Medicine Research and Evidence-Based Practice Committee. Psychosomatics 2014;55:109-22.
4. Ramanuj PP, Pincus HA. Collaborative care: enough of the why; what about the how? Br J Psychiatry 2019:1-4.
5. Insel TR. Treatment Development: the Past 50 Years. Director's Blog. Bethesda, MD: National Institute of Mental Health; 2011.




