Chronic Pain
Brain Imaging Shows We Can Unlearn Chronic Pain
Neuroanatomical changes observed with learning and unlearning of chronic pain.
Posted October 27, 2017
Two new studies, one published last month and another slated for publication in early 2018, confirm through brain imaging and other techniques, that pain that persists long after the physical injury that originally caused the pain has healed, is a type of learned behavior that can be “unlearned” through a variety of non-medical interventions.
For a September 2017 electronic pre-print of an article to appear later this year in the journal Psychological Medicine, Yoshino and colleagues of Hiroshima University Medical School examined the resting state functional magnetic resonance (rFMRI) of both chronic pain patients and healthy controls. rFMRI, shows which parts of the brain are intrinsically connected to each other by demonstrating correlated simultaneous activity among multiple brain regions. Brain regions that are wired together typically “fire” at the same time “rest” at the same time, because one of the brain regions presumably stimulates another through synaptic connections. Thus separated regions of the brain that exhibit correlated activity are said to belong to the same “Intrinsic Connectivity Network (ICN).
Yoshino’s research in 29 chronic pain sufferers and 30 healthy control subjects revealed abnormally high ICN connectivity within the “Dorsal Attention Network” (where consciously directed focal attention is thought to originate)—including structures such as the orbitofronal cortex and inferior parietal lobule— in chronic pain sufferers vs. healthy controls. This finding lead the authors to suggest that the brains of chronic pain suffers might rewire themselves when patients’ repeatedly focus attention on pain and/or anticipation of pain. Furthermore this rewiring could play a key role, according to Yoshino, in the continuance of pain after physical damage that caused the pain has healed.
Neuroscientists such as Dr. Waschulewski-Floruss of Eberhard-Karls University of Tuebingen in Germany have found that “learning” of chronic pain, and re-wiring of the brain, arises through the process of classical conditioning.
Here's how.
In his original experiments on classical conditioning in dogs, Pavlov noticed that dogs naturally salivated when they saw food. The food, in Pavlov’s example was an Unconditioned Stimulus (UCS) and the salivation an Unconditioned Response (UCR) to seeing the food. After Pavlov repeatedly paired the ringing of a bell with the presentation of food, the bell, even in the absence of food, became a Conditioned Stimulus (CS) that produced salivation. Salivation produced by a bell—not food--was called the Conditioned Response (CR).
This type of learning in dogs is associated with the formation of novel neural connections, where sensory inputs from the dog’s acoustic system, which did not originally stimulate parts of the dog’s brain that triggered salivation, grew new connections (or greatly strengthened existing connections) that enable the acoustic system to stimulate salivation.
The figure below represents how an injury could lead to “learned” chronic pain, and the formation of new neural pathways (“natural” pathways are shown in blue, learned pathways are depicted in red ), even after an injury is healed.
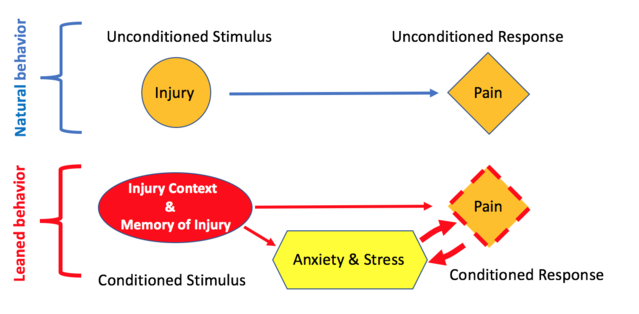
As shown in the figure, classical conditioning of chronic pain would occur as follows: The original physical injury is an unconditioned stimulus (UCS), the original pain from the injury is the unconditioned response (UCR), the conditioned stimulus (CS) is the memory of the events (context) surrounding the injury or obsessive worries about the pain, while the Conditioned response (CR) is the experience of pain in the presence of the CS (memory of injury and/or obsessive worries about the injury).
After pain has been “learned” in this way, a vicious circle is created, according to psychiatrist and pain specialist Joseph Hullett, in which the stress associated with anxiety about pain worsens the pain by altering the way pain control neurotransmitters such as norepinephrine and serotonin reduce pain. When pain worsens, anxiety grows worse, further increasing the pain …and so on.
But Pavlov’s original work provides a clue about how patients can “unlearn” the pain response shown in this figure and escape this vicious circle.
After training his dogs to salivate when they heard a bell, Pavlov rang the bell many times in the absence of food, so that eventually, dogs no longer salivated when they heard the bell. Such “unlearning” is called extinction.
If it were possible to stop chronic pain sufferers from focusing on their pain and memories of the injury that originally caused it, the pairing of these thoughts and memories with the experience of pain would end, and the learned response (pain) might decrease to extinction (as with conditioned salivation in Pavlov’s dogs).
In order to accomplish extinction of the learned pain response, Yoshino administered 12 weeks of Cognitive Behavioral Therapy (CBT), in which patients learned to control their thoughts, and to reduce their arousal level and anxiety associated with pain. This re-conditioning, decoupled thoughts, memories and anxieties about pain from the experience of pain, transforming a vicious circle into a virtuous circle, where lowered anxiety lead to lower arousal and stress, which in turn lead to lower pain, etc. In parallel, the rFMRI scans of CBT chronic pain sufferers began to look much more like those of healthy controls, indicating that CBT had rewired the brains of pain patients (eliminating or weakening the red “learned” pathways shown in the figure above).
Yoshino and colleagues concluded from these results that CBT helped chronic pain sufferers “unlearn” their pain by rewiring brain circuits in the Dorsal Awareness Network and other regions of the brain, such as dorsal posterior cingulate cortex, that were examined in study.
An article set to appear in the March 2018 issue of the journal Mindfulness by clinical psychologist Alice Shires and associates at the University of Sydney, reinforced Yoshino’s results, demonstrating that practicing a mindfulness interoceptive exposure task (MIET) for 15 days, also significantly reduced perception of pain in 15 chronic pain sufferers. In MIET, patients focus on bodily sensations of pain, consciously decomposing the discomfort into constituent sensations such as temperature, mass (how "heavy" does it seem), and motion. By breaking down the pain into its parts, patients “learn” a different relationship with pain, where pain transforms from being something constantly dreaded, into simple sensations that are noted, but then ignored.
Both Yoshino and Shires work demonstrate that-- at least in some cases where the physical injury has healed but pain from the injury persists—chronic pain can be “unlearned.” Further, Yoshino’s research suggests that such “unlearning” arises from anatomical rewiring of attention, memory and pain centers in the brain.
These are important findings because:
- They show that persistent pain in physically healed patients is not “all in their heads” but based upon anatomical changes within their nervous systems.
- They offer hope for 50 million adult chronic pain sufferers in the U.S. and many more worldwide.
- They show ways to significantly reduce health care costs nationwide. Treatment of chronic pain in the U.S. now costs in excess of $650 billion a year
- They offer non-pharmaceutical solutions to treating pain, that will reduce side effects, and medical mistakes (from prescription errors).
- They offer meaningful alternatives to opioids, potentially helping us cope with the opioid epidemic.
References
https://www.ncbi.nlm.nih.gov/pubmed/7829288
https://www.sciencedaily.com/releases/2012/09/120911091100.htm
http://americanpainsociety.org/about-us/press-room/nih-study-shows-prev…
https://www.cambridge.org/core/journals/psychological-medicine/article/…
https://opus.lib.uts.edu.au/handle/10453/118583
https://link.springer.com/article/10.1007/s12671-017-0823-x
http://www.scandinavianjournalpain.com/article/S1877-8860(17)30026-5/fu…
http://www.painphysicianjournal.com/linkout?issn=1533-3159&vol=20&page=…
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3715316/
https://www.webmd.com/pain-management/features/cognitive-behavioral#1




