Coronavirus Disease 2019
Skin Colour, Vitamin D Deficits and Disease Risks
Deficiency has been associated with multiple sclerosis and even COVID-19.
Posted October 15, 2020 Reviewed by Ekua Hagan
My previous blog post ("Vitamin D Is Essential for Human Reproduction") discussed the “sunshine vitamin” and emphasized the impacts of deficiency on reproductive health. But this topic is too big for one post. The fundamental interaction between skin colour, latitude, and Vitamin D was omitted. Moreover, readers’ comments highlighted additional diseases linked to deficiency, notably multiple sclerosis.
Vitamin D deficiency surveyed
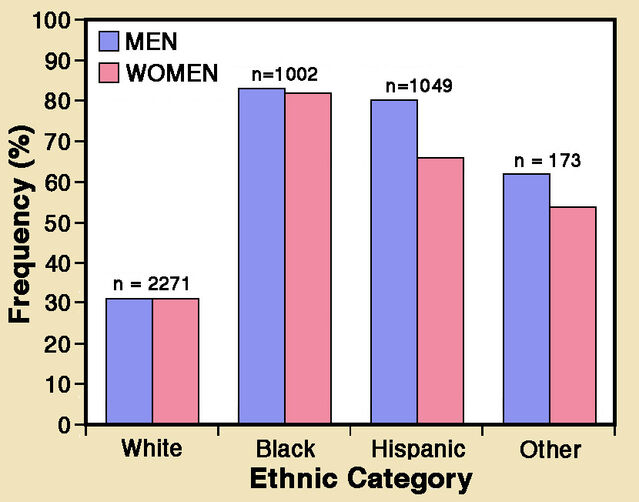
Vitamin D deficiency has long been a rampant pandemic. In 2011, Kimberly Forrest and Wendy Stuhldreher reviewed data from 2005-2006, almost 4,500 adults in the US National Health and Nutrition Examination Survey. Deficiency—defined as a blood level of 25-hydroxyvitamin D below 20 ng/m—was about 42% overall. Moreover, rates were much higher among minorities: 82% for African Americans and 69% for Hispanics.
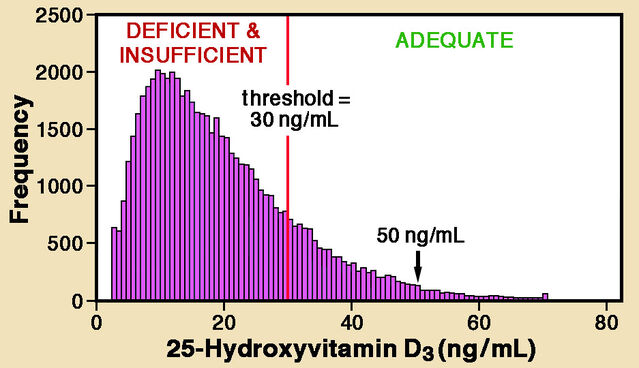
Five years later, Afrozul Haq and colleagues reviewed findings for a very different region: the United Arab Emirates (UAE). They analyzed 25-hydroxyvitamin D levels of almost 61,000 patients admitted to a single hospital in Abu Dhabi in 2012-2014. Half were UAE residents, while the others originated from 136 countries, mainly in the Middle East and Asia. Taking a higher threshold of 30 ng/mL, Haq and colleagues identified insufficient vitamin D levels in 82.5% of patients. Despite abundant sunshine, levels are strikingly low among Middle Eastern countries. Extreme deficiency is also far more common in women (26%) than men (18%), probably reflecting clothing traditions.
Vitamin D and skin colour
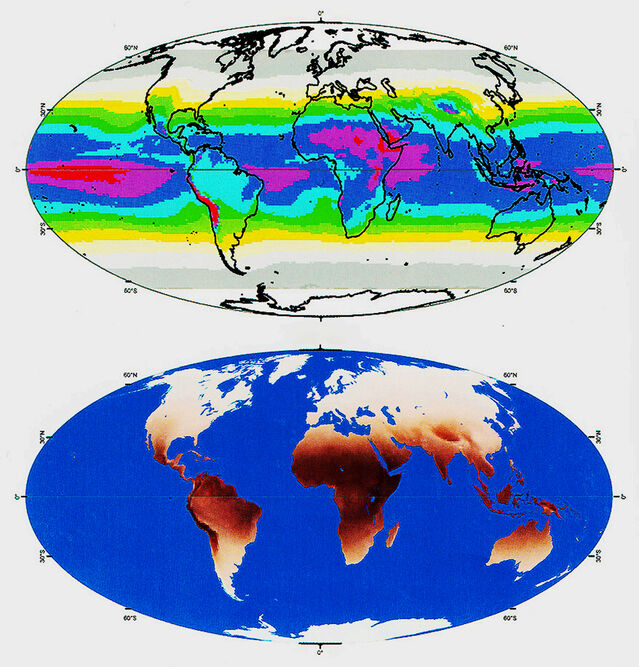
Triggering of vitamin D production in the skin by ultraviolet (UV) rays in sunlight, marked limitation at high latitudes, and a key rôle for human skin colour are well-established facts. But they are just part of a fascinating evolutionary story that a groundbreaking 2000 paper by Nina Jablonski and George Chaplin revealed. The crux is that natural selection, acting on variation in production of the pigment melanin, adjusts skin penetration by UV radiation.
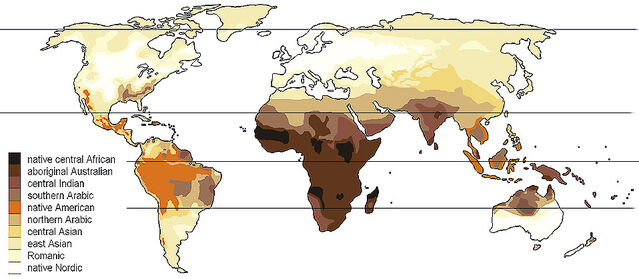
In an original approach, Jablonski and Chaplin used data on global UV levels from NASA remote sensing studies to determine the expected distribution of skin colours. Predicted and actual patterns of skin pigmentation matched very closely for resident human populations around the world. Skin colour is, of course, mainly associated with latitude. Inhabitants of tropical regions typically have dense pigmentation that gradually diminishes with increasing distance from the equator. But—as Jablonski’s 2006 book Skin: A Natural History explains—other factors intervene. For instance, a thinner atmosphere at high elevation, such as on the Tibetan plateau, permits greater penetration. Conversely, in equatorial rainforests denser cloud cover and humidity reduce incoming UV.
Because UV radiation is markedly reduced at high latitudes, paler skins with reduced blocking by melanin make sense. Why are skins darker in tropical regions? Jablonksi and Chaplin convincingly proposed two major negative risks of high UV radiation levels: destruction of folate and direct damage to DNA. Folate—a.k.a. vitamin B-9—is essential for human reproduction, especially during embryonic and fetal life, notably affecting nervous system development. In short, human skin colour is a compromise between preventing destructive effects of solar radiation and promoting vitamin D production.
Jablonksi and Chaplin also noted that worldwide women tend to have paler skin than men. They suggested that this might be an adaptation allowing pregnant or breastfeeding women to augment vitamin D production. Several authors have supported an alternative hypothesis that this difference is due to a universal male preference (sexual selection). But if that were the case, male/female difference should be greater at high latitudes because strong natural selection for dark skin should override male preference in tropical regions. In 2007, Lorena Madrigal and William Kelly reported test results showing that male/female skin colour differences are not correlated with latitude.
Vitamin D deficiency and multiple sclerosis
It has long been recognized that vitamin D is essential to develop and maintain healthy bones. But links between vitamin D and many human health issues have slowly emerged. A relatively new, startling example is multiple sclerosis (MS). This debilitating disease of the central nervous system is characterized by episodic deterioration of myelin sheaths around fast-conducting nerve fibres, causing accumulating neurological deficits. Over the past two decades, numerous studies have found an association between low blood levels of 25-hydroxyvitamin D and increased risk of developing MS. Moreover, patients with low 25-hydroxyvitamin D levels have poorer outcomes. However, several papers have questioned the success of treating MS with unusually high vitamin D doses.
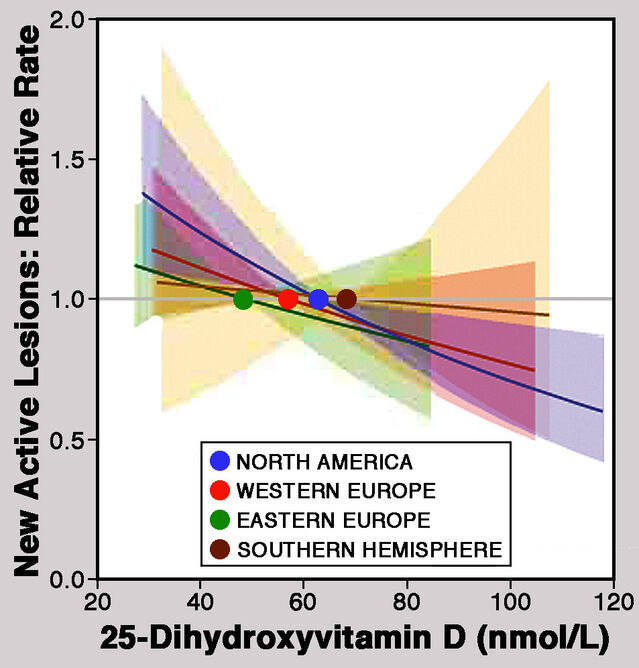
Seeking a more convincing test of the association between MS and vitamin D levels, Kathryn Fitzgerald and colleagues conducted a large-scale prospective study. They analyzed data from 26 countries for 1,500 patients with relapsing-remitting MS participating in the Betaferon Efficacy Yielding Outcomes of a New Dose trial. Patients were monitored for at least 2 years and magnetic resonance imaging (MRI) was used to quantify active lesions in the nervous system. Results published in 2015 revealed a significant decrease in the cumulative number of new lesions as blood levels of 25-hydroxyvitamin D increased. An increase of 20 ng/mL in circulating levels of 25-hydroxyvitamin D was associated with a decrease in the rate of appearance of new lesions by one third. Fitzgerald and colleagues concluded that their findings “suggest that adequate vitamin D status is an important determinant of MS activity not only early in the disease course but also several years after the diagnosis” and that “individuals with MS may benefit from vitamin D levels above those currently considered by many to be sufficient in healthy adults."
An enigma and a brand new example
An extensive list of links between vitamin D and human health issues now exists. Leonard Greenfield’s 2015 very informative book Vitamin D Deficiency in Modern Humans and Neanderthals listed 55 examples and more have been added since.
But a mystery remains: In the USA, typical amounts of vitamin D in breast milk are way below a baby’s needs. In 2016, Susanna Streym and colleagues reported findings for infants at three ages after birth—2 weeks, 4 months, and 9 months. Breast milk analyses showed that infants received an average of only 77 International Units of vitamin D per day, less than one-fifth of the recommended amount. Moreover, milk vitamin D content varied greatly between seasons. Yet advising parents to avoid exposing infants directly to sunlight potentially leaves exclusively breastfed babies entirely dependent on vitamin D in breast milk! Encouragingly, Streym and colleagues found that vitamin D supplementation does boost levels in breast milk.
Topically, very recent information links vitamin D status to the ongoing COVID-19 pandemic. Two preliminary reports, still under peer review, provide different kinds of evidence. The first, by David Meltzer and colleagues, reports that positive COVID-19 test results are significantly associated with vitamin D status. For deficient individuals, the risk of a positive diagnosis was almost doubled compared to those with adequate vitamin D levels. The second, by Aduragbemi Faniyi and colleagues, reported on 400 UK healthcare workers isolated because of possible COVID-19 symptoms, 55% of whom tested positive. Infection was significantly more likely with vitamin D deficiency (72%) than with sufficiency (51%).
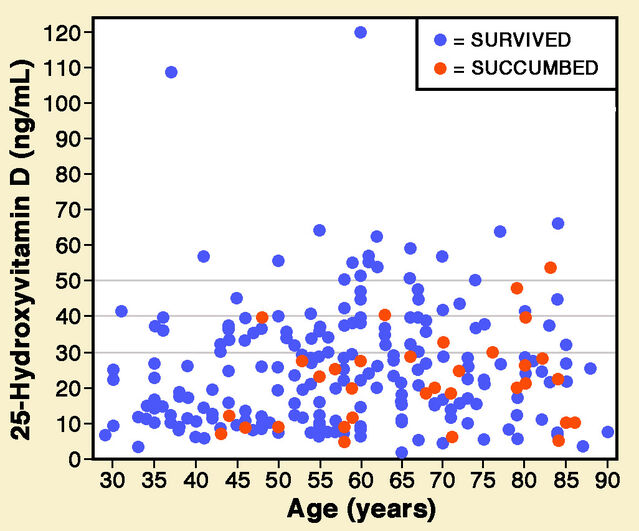
A peer-reviewed paper just published by Zhila Maghbooli and colleagues provides compelling evidence. They investigated the association between serum 25-hydroxyvitamin D levels and COVID-19 mortality in hospital data for 235 patients. Only 9.7% of patients with levels of 25-hydroxyvitamin D above 30 ng/mL died, compared to 20% below that threshold. Data presented by Maghbooli and colleagues shows that only 19 patients had levels above 50 ng/mL, only one of whom died (around 5%). Vitamin D may provide dose-related protection.
References
Faniyi, A.A., Lugg, S.T., Faustini, S.E., Webster, C., Duffy, J.E., Hewison, M., Shields, A., Nightingale, P., Richter, A.G. & Thickett, D.R. (2020) Vitamin D status and seroconversion for COVID-19 in UK healthcare workers who isolated for COVID-19 like symptoms during the 2020 pandemic. medRxiv 10.05.20206706:1-22.
Fitzgerald, K.C. et al. (2015) Association of vitamin D levels with multiple sclerosis activity and progression in patients receiving interferon beta-1b. JAMA Neurology 72:1458-1465.
Forrest, K.Y.Z. & Stuhldreher, W.L. (2011) Prevalence and correlates of vitamin D deficiency in US adults. Nutrition Research 31:48-54.
Greenfield, L.O. (2015) Vitamin D Deficiency in Modern Humans and Neanderthals. Colorado: Outskirts Press.
Haq, A., Svobodová, J., Imran, S., Stanford, C. & Razzaque, M.S. (2016) Vitamin D deficiency: A single centre analysis of patients from 136 countries. Journal of Steroid Biochemistry & Molecular Biology 164:209-213.
Holick, M.F. & Chen, T.C. (2008) Vitamin D deficiency: a worldwide problem with health consequences. American Journal of Clinical Nutrition 87(Suppl):1080S-1086S.
Jablonski, N.G. (2006) Skin: A Natural History. Berkeley CA: University of California Press.
Jablonski, N.G. & Chaplin, G. (2000) The evolution of human skin coloration. Journal of Human Evolution 39:57-106.
Jablonski, N.G. & Chaplin, G. (2010) Human skin pigmentation as an adaptation to UV radiation. Proceedings of the National Academy of Sciences U.S.A. 107 (Suppl. 2):8962-8968.
Maghbooli, Z., Sahraian, M.A., Ebrahimi, M., Pazoki, M., Kafan, S., Tabriz, H.M., Hadadi, A., Montazeri, M., Nasiri, M., Shirvani, A. & Holick, M.F. (2020) Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection. PLoS One 15(9),e0239799:1-13.
Meltzer, D.O., Best, T.J., Zhang, H., Vokes, T., Arora, V. & Solway, J. (2020) Association of Vitamin D Deficiency and Treatment with COVID-19 Incidence. medRxiv 05.08.20095893:1-22.
Streym, S., Højskov, C.S., Møller, L.K., Heickendorff, L., Vestergaard, P., Mosekilde, L. & Rejnmark, L. (2016) Vitamin D content in human breast milk: a 9-mo follow-up study. American Journal of Clinical Nutrition 103:107-114.




