Health
Vitamin D Is Essential for Human Reproduction
We need the sunshine vitamin for much more than healthy bones.
Posted September 15, 2020

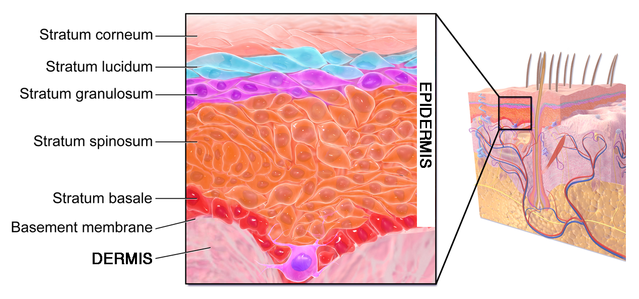
Every schoolchild learns that vitamin D is essential for proper bone development. Deficiency leads to rickets, a classical childhood affliction with soft, deformed bones resulting in bowed legs. The main biologically active form is vitamin D3, dubbed the “sunshine vitamin” because ultraviolet rays in sunlight trigger its formation in the surface layer of the skin (epidermis).
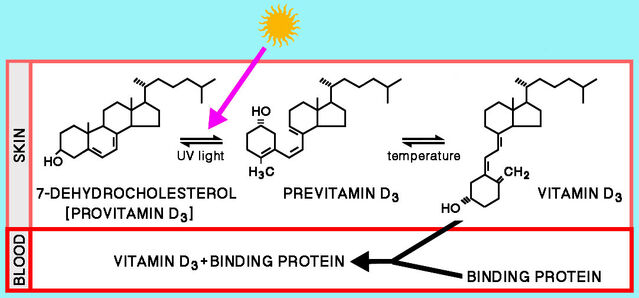
Short-wavelength ultraviolet-B rays convert provitamin-D3 (a form of cholesterol) into previtamin-D3, which is then transformed into vitamin D3 (cholecalciferol). Vitamin D3 produced in the skin or obtained in the diet is further converted in the liver to 25-hydroxyvitamin D3 (the main form in the bloodstream) and then in the kidney to the bioactive 1,25-dihydroxyvitamin D3.
Various foods (particularly fish livers and egg yolks) contain vitamin D3, but under optimal conditions, enough can be formed in human skin to meet bodily needs. So it is not really a “vitamin” — which must be ingested in food — and it actually acts like a hormone. Correspondingly, it has slowly emerged that vitamin-D3 is vital for human reproductive health.
Vitamin D: Sunshine and skin
Vitamin D requirements can, in principle, be met by sunlight triggering production in human skin. But two major obstacles exist: clothing that often shields most skin from sunlight and the effect of latitude.
As distance from the equator increases, total sunlight gradually declines. Moreover, seasonal changes generate marked variation — especially at high latitudes. In mid-winter, people wearing cold-weather clothing at high latitudes receive too little sunlight to produce vitamin D3. In 1988, Ann Webb and colleagues reported that no previtamin D3 at all was produced in human skin exposed to sunlight on cloudless days in November to February in Boston, MA (42.2°N). Further north in Edmonton, Canada (52°N), vitamin D3 production was suppressed from October through March, whereas sunlight yielded vitamin D3 even in mid-winter down south (below 34°N).
In 1992, Lois Matsuoka and colleagues reported clear evidence that clothing blocks vitamin D3 production. They measured the effects of widely used black or white fabrics (cotton, wool, polyester). Black wool blocked UV-B light most (nearly completely) and white cotton least (around half). Importantly, however, in laboratory tests, irradiation with simulated sunlight through any fabric failed to trigger conversion of provitamin D3 to previtamin D3. Moreover, full-body UV-B irradiation of volunteers wearing jogging clothes in those fabrics or ordinary street clothing did not raise blood levels of vitamin D3 even at high exposure.
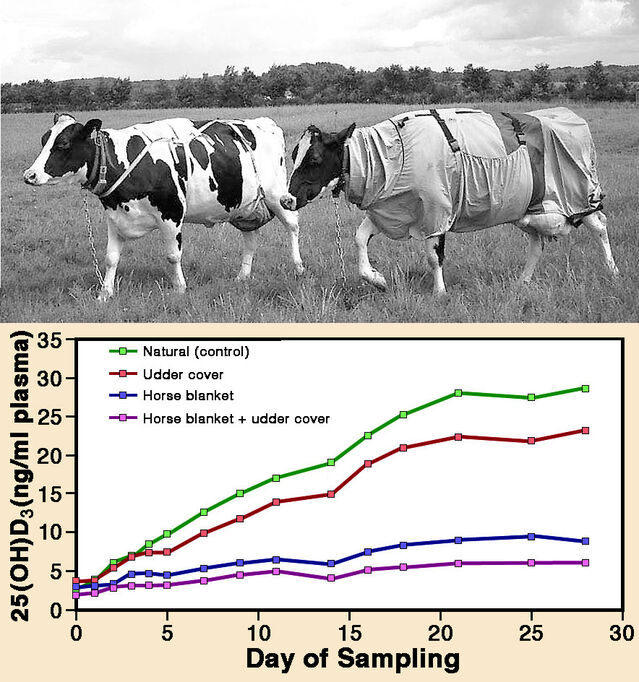
It has often been stated that, like clothing, mammal fur and bird feathers block UV-light. It was therefore suggested that vitamin D3 might either be formed on fur/feathers and then ingested during grooming, or produced exclusively in exposed skin areas such as the face. But those explanations had barely been tested before 2010, when Lone Hymøller and Søren Krogh Jensen reported results from a neat experiment with cows.
They measured levels of 25-hydroxyvitamin D3 in cows with body areas covered to differing extents with light-blocking fabric: (1) body covered with a horse blanket; (2) udder alone covered; (3) both body and udder covered; (4) body and udder uncovered (control condition). All cows were let out to pasture for four weeks in July/August, for five hours in the middle of every day. At the end of the study, blood levels of 25-hydroxyvitamin D3 were highest in uncovered cows and lowest in cows with both body and udder covered. Cows with only the udder covered ranked second, while cows with a blanket covering the body ranked third. So sunlight evidently penetrates cow fur sufficiently for vitamin D3 to be produced over the entire body surface.
It is also known that sunscreens — designed to protect against cancer by blocking UV-B light entry into the skin — suppress vitamin D3 production. In 1987, Lois Matsuoka and colleagues reported results of experiments with para-aminobenzoic acid. With four human test subjects anointed with that sunscreen, a low dose of UV radiation approximately tripled blood levels of vitamin D3, but levels were increased almost 18-fold in four control subjects without sunscreen. Matsuoka and colleagues also found that sunscreen prevented conversion of provitamin D3 to previtamin D3 in laboratory tests with human skin slices.
Vitamin D deficiency and reproductive health
Twenty-five years ago, Michael Holick noted that vitamin D deficiency had reached epidemic status, afflicting tens of millions of people in the USA alone. Ten years later he stated that about 36% of otherwise healthy young adults reportedly had vitamin deficiency, with even higher frequencies in Europe. Serious impacts on reproductive health have emerged. In one notable paper in 2000, Keiko Kinuta and colleagues reported research results for mutant mice with cells lacking Vitamin D receptors. Major effects on oestrogen production were identified. Womb development and ovarian follicle production were impaired in females, while sperm count and motility were reduced in males.
Several effects of low vitamin D3 levels during human pregnancy have also been recognized. In 2013, a systematic review by Fariba Aghajafari and others assessed adverse pregnancy outcomes associated with low blood levels of 25-hydroxyvitamin D3. These authors surveyed results from 31 studies published from 1980 to 2012, averaging 600 subjects each. With below-par blood levels of 25-hydroxyvitamin D3, risks were significantly increased by 85% for birth of undersized infants, by 80% for pre-eclampsia, and by 50% for gestational diabetes.
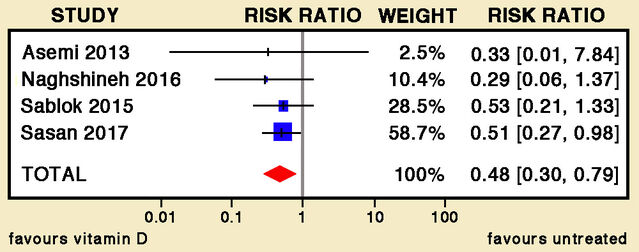
Addressing the issue of intervention to offset deficiency, in 2019 Cristina Palacios and colleagues reviewed the effects of oral supplementation with Vitamin D3 during pregnancy. Their comprehensive combined analysis of 22 trials involving almost 4000 women yielded valuable conclusions. Risks for pre‐eclampsia, gestational diabetes, and low birth weight were approximately halved with vitamin D3 supplementation. Moreover, the risk of severe postpartum haemorrhage was reduced by about a third.
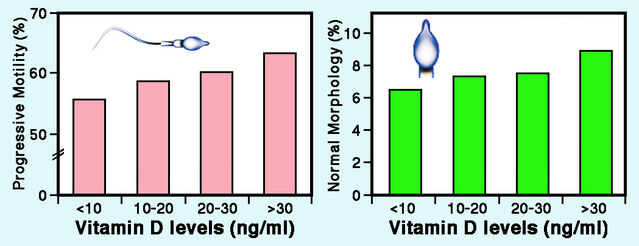
Following previous reports indicating that vitamin D deficiency adversely influences semen (e.g. by Kinuta and co-authors), a 2011 paper by Mart Blomberg Jensen and colleagues examined the relationship between blood levels of 25-hydroxyvitamin D3 and sperm function in Danish men. As expected for a high northern latitude, marked seasonal differences emerged: Average levels were almost twice as high in summer as in winter, with intermediate values in spring and autumn. Regardless of season, all semen traits were positively correlated with circulating levels of 25-hydroxyvitamin D3, although results were statistically significant only for sperm motility.
A broader perspective
Cholesterol — the precursor for vitamin D3 production — is a steroid, so links to hormonal processes are hardly surprising. Surveys have reported various links between vitamin D3 deficiency and reproductive health, although confident assessment will require randomized control trials. One consistent finding is the increased incidence of pre-eclampsia, a serious medical condition affecting 1 in 20 pregnancies worldwide. As long as doses are not excessive, available evidence surely justifies active intervention as a precautionary measure to avoid deficiency during pregnancy. Physicians now widely recognize this, but many pregnant women fail to take the recommended supplements.
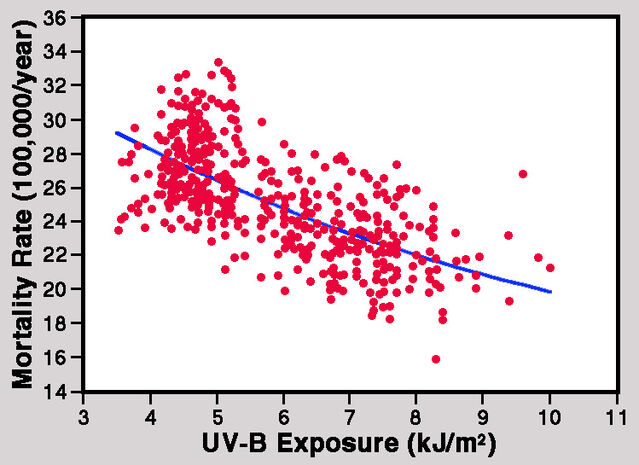
Similar precautions are appropriate with evidence linking vitamin D deficiency to various cancers. Studies have repeatedly revealed a connection with colon cancer, and preliminary evidence indicates links with certain reproductive cancers — notably of the breast and prostate. A 2002 paper by William Grant has, for instance, convincingly documented an inverse relationship between mortality rates for breast cancer and ambient UV-B levels. With good nutrition, exposure to sunlight can yield enough additional vitamin D3, but modern living conditions have increasingly led to serious side-effects of deficiency.
Acknowledgment
I am very grateful to Professor Søren Krogh Jensen for generously approving the use of an adapted image combining the two figures in his 2010 paper co-authored with Dr. Lone Hymøller.
References
Aghajafari, F., Nagulesapillai, T., Ronksley, P.E., Tough, S.C., O'Beirne, M. & Rabi, D.M. (2013) Association between maternal serum 25-hydroxyvitamin D level and pregnancy and neonatal outcomes: systematic review and meta-analysis of observational studies. British Medical Journal 346,f1169:1-14.
Blomberg Jensen, M., Bjerrum, P.J., Jessen, T.E., Nielsen, J.E., Joensen, L.N., Olesen, I.A., Petersen, J.H., Juul, A., Dissing, S. & Jørgensen, N. (2011) Vitamin D is positively associated with sperm motility and increases intracellular calcium in human spermatozoa. Human Reproduction 26:1307-1317.
Grant, W.B. (2002) An estimate of premature cancer mortality in the U.S. due to inadequate doses of solar ultraviolet-B radiation. Cancer 94:1867-1875.
Holick, M.F. (2005) The vitamin D epidemic and its health consequences. Journal of Nutrition 135:2739S-2748S.
Holick, M.F. (2006) High prevalence of vitamin D inadequacy and implications for health. Mayo Clinic Proceedings 81:353-373.
Holick, M.F. (2010) The Vitamin D Solution: A 3-Step Strategy to Cure Our Most Common Health Problems. New York: Hudson Street Press (Penguin Group).
Hymøller, L. & Jensen, S.K. (2010) Vitamin D3 synthesis in the entire skin surface of dairy cows despite hair coverage. Journal of Dairy Science 93:2025-2029.
Kinuta, K, Tanaka, H., Moriwake, T., Aya, K., Kato, S. & Seino, Y. (2000) Vitamin D is an important factor in estrogen biosynthesis of both female and male gonads. Endocrinology 141:1317-1324.
Matsuoka, L.Y., Ide, L., Wortsman, J., MacLaughlin, J.A. & Holick, M.F. (1987) Sunscreens suppress cutaneous vitamin D3 synthesis. Journal of Clinical Endocrinology & Metabolism 64:1165-1168.
Matsuoka, L.Y., Wortsman, J., Dannenberg, M.J., Hollis, B.W., Lu, Z. & Holick, M.F. (1992) Clothing prevents ultraviolet-B radiation dependent photosynthesis of vitamin D3. Journal of Clinical Endocrinology & Metabolism 75:1099-1103.
Palacios, C., Kostiuk, L.K. & Peña-Rosas, J.P. (2019) Vitamin D supplementation for women during pregnancy. Cochrane Database Systematic Reviews 2019(7) Art No CD008873:1-146.
Webb, A.R., Kline, L. & Holick, M.F. (1988) Influence of season and latitude on cutaneous synthesis of vitamin D3: exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin. Journal of Clinical Endocrinology & Metabolism 67:373-378.




