Psychiatry
Psychosomatic Illness and the Mind-Body Problem
What these disorders tell us about the nature of mental illness.
Posted December 29, 2021 Reviewed by Ekua Hagan
Key points
- Psychosomatic disorders have historically been conceptualized as psychological problems manifesting as physical symptoms.
- Modern approaches attempt to integrate psychological and biological understandings of psychosomatic disorders.
- Psychosomatic disorders demonstrate the importance of a comprehensive biopsychosocial model.
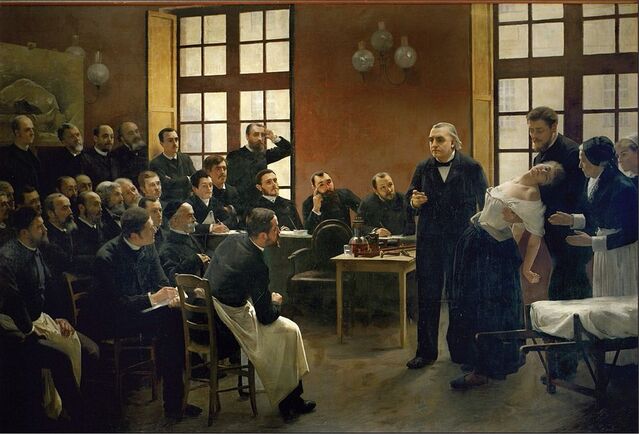
The notion that psychological problems can manifest as physical disorders or symptoms predates the founding of modern scientific psychiatry in the late 1800s. Indeed, it is an idea as old as medicine itself. For centuries, these types of conditions were labeled hysteria, a term that McHugh and Slavney (1998), writing in the second edition of their now-classic textbook The Perspectives of Psychiatry, call "one of the great words of psychiatry—right up there with mania, delirium, and dementia."
In the latter half of the twentieth century, "hysteria" fell out of favor, in part because it had for too long been associated with outdated and misogynistic notions about its cause—namely, a displaced or "wandering" uterus. Other terms soon came to replace it, such as "somatoform disorder" and now "somatic symptom disorder," though the latter term, introduced in DSM-5, refers problematically to an amalgamation of various types of problems (see Frances, 2013).
For decades, these conditions have also been described as "psychogenic illnesses" or "psychosomatic disorders," owing to the idea that psychological factors (psycho-) are causative (-genic) of bodily (somatic) symptoms.
Exploring the mind-body problem
The concept of psychosomatic illness sheds some light on a question that has plagued philosophers for centuries, namely, the mind-body problem. Generally, the mind-body problem refers to the question of how to address the relationship between mental phenomena and neural or physical phenomena. Psychosomatic disorders also demonstrate the importance of the biopsychosocial model (Engel, 1977), a theory that has guided psychiatric teaching and practice for the past four decades.
When it comes to conversion disorder, a form of psychosomatic illness now also referred to as functional neurological symptom disorder, a shift from predominantly psychological and psychodynamic models to neurologically informed models has been observed. For instance, the Functional Neurological Disorder (FND) Clinic at Massachusetts General Hospital describes FND as "a problem largely impacting the functioning of the brain" (Massachusetts General Hospital, 2021).
This shift reflects a broadening recognition of the fact that psychological processes are also fundamentally physiological ones—a point recognized even by Freud, who was trained as a neurologist and neuroanatomist. While it is true that psychological and social forces weigh considerably in the development of psychosomatic disorders, these factors are also inherently biological ones, and growing evidence suggests biological dysfunction in these conditions (Bègue, Adams, Stone, & Perez, 2019).
A 2019 article in The Journal of Neuropsychiatry and Clinical Neurosciences explored the relationship between the psychoanalytic model of conversion and recent findings on the biology of functional neurological symptom disorder. It concluded that the conversion concept is consistent with the neuroscientific findings and that psychological and neurological models of the condition can be reconciled within a single account of FND that can begin to resolve the dualistic mind-body dichotomy (Cretton, Brown, LaFrance, & Aybek, 2019).
The authors write, "Our brief review suggests that both [biological and psychological] approaches [to conversion disorder] are appropriate, because they are both looking at the same entity from different angles, using different lenses and methods. To focus on one at the expense of the other, is to lose sight of the harmony between these accounts and the potential insights that each has to offer the other" (Cretton, Brown, LaFrance, & Aybek, 2019, p. 30). They add, "Ultimately, psychological processes have physiological substrates, and a comprehensive account of FND has to describe both" (p. 30).
The need for a pluralistic psychiatry
Such findings highlight the importance of pluralism in the conceptualization of psychiatric disorders, which are influenced by a combination of biological (and genetic), psychological, and social factors. To quote the great psychiatrist-psychoanalyst Silvano Arieti, "[Psychiatric] theoreticians should be open to all vistas and should work toward constructing bridges between equally plausible orientations. No reductionism of any kind but a pluralistic approach must prevail in psychiatry" (Arieti, 1969).
It is in this spirit that researchers and theoreticians continue to explore the complex relationship between brain and mind and its relevance to the understanding of psychosomatic and other psychiatric disorders.
References
Arieti, S. (1969). The present status of psychiatric theory. International Journal of Psychiatry, 8(3), 619-629.
Bègue, I., Adams, C., Stone, J., & Perez, D. L. (2019). Structural alterations in functional neurological disorder and related conditions: A software and hardware problem? Neuroimage. Clinical, 22, 101798.
Cretton, A., Brown, R. J., LaFrance, C., & Aybek, S. (2019). What does neuroscience tell us about the conversion model of functional neurological disorders? The Journal of Neuropsychiatry and Clinical Neurosciences, 32(1), 24-32.
Engel, G. (1977). The need for a new medical model: A challenge for biomedicine. Science, 196, 129-136.
Frances, A. (2013). The new somatic symptom disorder in DSM-5 risks mislabeling many people as mentally ill. BMJ (Clinical research ed.), 346, f1580.
Massachusetts General Hospital. (2021). Basics of FND. Massachusetts General Hospital. https://www.massgeneral.org/neurology/treatments-and-services/functiona…
McHugh, P. R., & Slavney, P. R. (1998). The perspectives of psychiatry (2nd ed.). Johns Hopkins University Press.


