Health
Are There Symptoms from Exposure to Environmental EMR?
What does research say about possible symptoms of EHS?
Posted October 20, 2019
Change always produces some fear, and, as the digital age gathers pace, new fears are developing. One concerns the potential relationship between low-frequency Electromagnetic Radiation (EMR), such is used to drive mobile devices, and Electromagnetic Hypersensitivity Syndrome (EHS). Unfortunately, while there is enough evidence to provoke concerns in the public about physical and psychological symptoms, and to prompt the European Economic and Social Committee (EESC) to recognise this distress as 'real,' there is not enough evidence to allay these fears. Given this, what is known about the extent to which EHS affects people, and what symptoms can it produce in their physical and mental states?
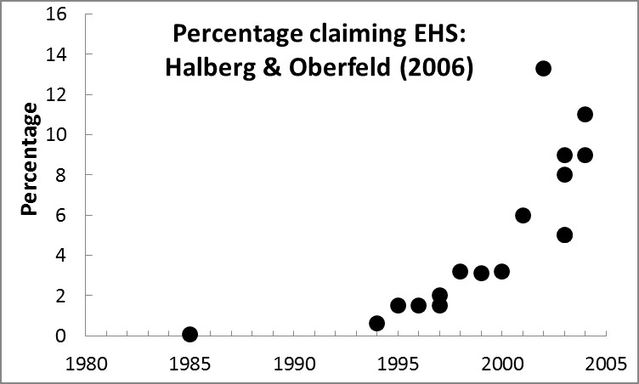
It is estimated that EHS causes distress and loss of quality of life for between 3% and 5% of the European population (i.e. between 22 and 37 million people; EESC, 2015). Moreover, increasing numbers of individuals are claiming that they experience EHS, in one form or another (see Figure 1). Observational studies have noted associations between a wide range of symptoms and presumed exposure to environmental non-ionising EMR1,2. These studies, typically, examine the correlation between symptoms and proximity to base stations3, or levels of mobile phone usage4. Unfortunately, as has often been repeated, correlation is not causation, and it is difficult to get definitive evidence of a causal link.
The reported symptoms of EHS can involve serious conditions, after long-term EMR exposure, as well as reversible symptoms, after shorter-term exposure1. The International Agency for Research on Cancer classified electromagnetic fields (EMFs) as being possibly carcinogenic for humans, and placed EMFs in the ‘Group 2B’ category of carcinogens. This category is employed when a causal association between a stressor and cancer is considered credible, but when there is insufficient evidence available to rule out the impact of chance, bias, or confounding factors with reasonable confidence5.
In addition to a wide range of cancers1,2, low-frequency non-ionising EMR exposure has been linked to other health problems, such as: asthma6, diabetes7, multiple sclerosis8, and reproductive dysfunction9. Furthermore, a number of neuropsychiatric and central nervous system conditions, such as: Alzheimer disease10, anxiety11, attention-deficit hyperactivity disorder1, autism spectrum disorder12, and depression13, have been associated with EMR exposure. Any putative associations between EMR and disease are of concern, because many of the conditions linked to environmental EMR have, themselves, shown an increase in prevalence over the last 20 years, and represent a substantial burden on health care resources. For example, the number of young people with depression has nearly doubled14, and sleep disturbances have risen sharply15. Whether these occurrences are linked causally to EMR, or not, even in part, remains completely unclear.
Although rises in condition prevalence have been linked by some, at least in part, to increased EMR exposure1, in the absence of causal evidence obtained through controlled experiments, this suggestion is impossible to even begin to verify. This is a critical point, as, if links to environmental triggers for these conditions were to be established, or dismissed, this would enable appropriately-targeted measures to be taken to reduce disease burden and improve public health – which may, or may not, involve a focus on environmental EMR. For this reason, the potential EMR link to disease needs investigation.
Health relationships with environmental EMR-exposure tend to be with single diseases, or apparently random symptom sets. Apart from these links, the most common symptoms self-reported by those who claim EHS, as a result of EMR exposure, are sleep disturbances, headaches, fatigue/tiredness, nausea, skin burning, dysesthesia, dizziness, irritability, loss of appetite/body weight, concentration and attention dysfunction, and memory changes (see Table 1). However, if EHS is to be accepted as a disease/syndrome, then it must involve clusters of multiple symptoms, in addition to, or separate from, other identifiable diseases1,2. This has not yet been established, leaving open the possibility that these conditions are not EMR-related.

Despite these cautions, there are theoretical reasons not to exclude the possibility of environmental non-ionising EMR impacting disease. Although the suggested conditions show a huge range of symptomatic differences from each other, many are related to biological systems hypothesised as being negatively affected by EMR exposure1,10. Evidence has been obtained from nonhuman studies and tissue cultures that EMR will affect histamine-related inflammatory responses10, which are implicated in diseases, such as asthma and some ASD. Additionally, EMR is taken to impact voltage-activated calcium gate channels2, which are widespread throughout the nervous system, and are related to many neuropsychiatric conditions. In line with these suggestions, a range of physiological markers, such as elevation of heat shock proteins16, melatonin reduction17, oxidative stress10, altered cerebral blood flow18, and increased inflammatory markers10, have all been noted in those with EHS. However, no single biological marker has been found to predict EHS19.
Unfortunately, while many of these conditions and claimed associations with environmental EMR are of great concern to the public and public-health officials, current research does not provide strong enough evidence, either way, relating to any adverse health effects from non-ionising EMF. In fact, there are numerous theoretical issues that have not been adequately addressed by current research. For example, as noted above, a central stumbling block is that it is unclear whether EHS distress is causally related to EMR exposure19, and the potential mechanisms of such a relationship remain unresolved1,2,10.
As a consequence of these gaps in knowledge, problems with the acceptance of EHS as a ‘real’ disorder have emerged, and have retarded the development of an approach that can help with this critical contemporary issue. Given these concerns, both the European Economic and Social Committee and the World Health Organisation have stressed that further research is essential to accumulate evidence concerning any potential health impact from EMR exposure. Such advice is imperative to follow: We know the consequences for public health of not addressing concerns about safety seriously enough, and of not vigorously addressing such concerns through public forums (witness measles), allowing poorly addressed fears, or poorly researched technology, to drive behavior. If EHS is a ‘real’ phenomenon, causally related to non-ionising EMR, then we need to know it. If it is not, then we need to be able to say why.
References
1. Belyaev, I., Dean, A., Eger, H., Hubmann, G., Jandrisovits, R., Johansson, O., ... & Moshammer, H. (2015). EUROPAEM EMF Guideline 2015 for the prevention, diagnosis and treatment of EMF-related health problems and illnesses. Reviews on Environmental Health, 30, 337-371.
2. Pall, M.L. (2015). Microwave frequency electromagnetic fields (EMFs) produce widespread neuropsychiatric effects including depression. Journal of Chemical Neuroanatomy, 75, 41-53.
3. Abdel-Rassoul, G., El-Fateh, O.A., Salem, M.A., Michael, A., Farahat, F., El-Batanouny, M.A., & Salem, E. (2007). Neurobehavioral effects among inhabitants around mobile phone stations. Neurotoxicology, 28, 434–440.
4. Chiu et al. (2014). Mobile phone use and health symptoms in children. J Formos Med Assoc., Aug 9, pii: S0929-6646(14)00207-1.
5. WHO (2014). Electromagnetic fields and public health: mobile phones. Fact sheet N°193: WHO.
6. Genuis, S.J. (2008). Fielding a current idea: exploring the public health impact of electromagnetic radiation. Public Health, 122(2), 113-124.
7. Yurekli, A. I., Ozkan, M., Kalkan, T., Saybasili, H., Tuncel, H., Atukeren, P., ... & Seker, S. (2009). GSM base station electromagnetic radiation and oxidative stress in rats. Electromagnetic Biology and Medicine.
8. Havas, M. (2006). Electromagnetic hypersensitivity: biological effects of dirty electricity with emphasis on diabetes and multiple sclerosis. Electromagnetic Biology and Medicine, 25(4), 259-268.
9. Hardell, L., Eriksson, M., Carlberg, M., Sundstrom, C., Mild, K.H. (2005). Use of cellular or cordless telephones and the risk for non-Hodgkin’s lymphoma. Int Arch Occup Environ Health, 78, 625–32.
10. Belpomme, D., Campagnac, C., & Irigaray, P. (2015). Reliable disease biomarkers characterizing and identifying electrohypersensitivity and multiple chemical sensitivity as two etiopathogenic aspects of a unique pathological disorder. Reviews on Environmental Health, 30(4), 251-271.
11. Johansson A., et al. (2010). Symptoms, personality traits, and stress in people with mobile phone-related symptoms and electromagnetic hypersensitivity. Journal of Psychosomatic Research, 68(1), 37–45.
12. Mortazavi, G., Haghani, M., Rastegarian, N., Zarei, S., & Mortazavi, S. M. J. (2016). Increased release of mercury from dental amalgam fillings due to maternal exposure to electromagnetic fields as a possible mechanism for the high rates of autism in the offspring: introducing a hypothesis. Journal of Biomedical Physics & Engineering, 6(1), 41.
13. Bortkiewicz, A., Zmyslony, M., Szyjkowska, A., & Gadzicka, E. (2004). Subjective symptoms reported by people living in the vicinity of cellular phone base stations: review. Med. Pr., 55, 345–351.
14. Hagell, A. (2012) Changing Adolescence: Social trends and mental health. Bristol: Policy.
15. Rowshan, R.A., Bengtsson, C., Lissner, L., Lapidus, L., & Bjorkelund, C. (2010). Thirty-six-year secular trends in sleep duration and sleep satisfaction, and associations with mental stress and socioeconomic factors--results of the Population Study of Women in Gothenburg, Sweden. J Sleep Res., 19(3), 496–503.
16. French, P.W., Penny, R., Laurence, J.A., & McKenzie, D.R. (2001). Mobile phones, heat shock proteins and cancer. Differentiation, 67(4–5), 93–7.
17. Altpeter, E., Battaglia, M., Bader, A., Pluger, D., Minder, C.E., & Abelin, T. (2000). Ten years’ experience with epidemiological research in the vicinity of the short-wave broadcasting area Schwarzenburg: What does the story tell us?. http://www.salzburg.gv.at/Proceedings_%2819%29_Altpeter.pdf.
18. Oscar, K.J., Gruenau, S.P., Folker, M.T., & Rapoport, S.I. (1981). Local cerebral blood flow after microwave exposure. Brain Research, 204(1), 220–5.
19. Genuis, S. J., & Lipp, C. T. (2012). Electromagnetic hypersensitivity: fact or fiction?. Science of the Total Environment, 414, 103-112.


