Long Covid
POTS and Long COVID: A Dizzying Partnership
What we understand about the relationship between long COVID and POTS.
Posted July 8, 2023 Reviewed by Gary Drevitch
Key points
- Postural orthostatic tachycardia syndrome, a form of dysautonomia, often develops after COVID-19 illness.
- Recent research shows that 30 percent of long-haulers meet criteria for POTS.
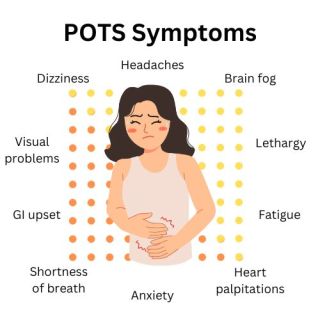
- POTS causes symptoms including lightheadedness, fainting, heart palpitations, and shakiness.
- Self-management of POTS is possible with simple lifestyle changes.
Long-haulers struggle with a multitude of lingering and often disabling symptoms. One particularly troubling cluster of symptoms is autonomic nervous system dysfunction. In fact, a recent international survey revealed that 67 percent of long-haulers report moderate to severe autonomic dysfunction (i.e., dysautonomia). Unfortunately, one of the most common forms of dysautonomia among long-haulers—Postural Orthostatic Tachycardia Syndrome, or POTS—is infrequently recognized and diagnosed.
In fact, a survey conducted by Dysautonomia International found that the average diagnostic delay for a POTS patient was over 5 years. Unfortunately, 60 percent of these individuals were originally told the symptoms were “all in your head” and more that 25 percent of them visited at least 10 doctors before finally receiving a POTS diagnosis.
What is the connection between long COVID, dysautonomia, and the new onset of POTS? This post aims to answer that question.
The autonomic nervous system (ANS) is responsible for vital involuntary bodily functions, such as breathing and digestion. The ANS can be divided into three separate divisions:
- Parasympathetic (responsible for “rest and digest” bodily processes)
- Sympathetic (governs “fight or flight” processes)
- Enteric (manages how the body digests food)
While the underlying causal factors remain speculative at this point, we do know that COVID-19 infection can disrupt the normal processes of the ANS. It has been hypothesized that the COVID-19 virus may invade the ANS through a variety of means including neuronal and hematological (e.g., crossing the blood brain barrier) routes, autoimmune dysfunction, and persistent systemic inflammation.
What is dysautonomia?
When our autonomic nervous system doesn’t function as it should, it can cause a broad spectrum of symptoms. We may experience GI problems like constipation, heart palpitations, lightheadedness, heat intolerance, and excessive thirst or fatigue.
Viral infections like COVID-19 may cause a specific type of dysautonomia: POTS. Researchers are consistently finding a strong link between COVID-19 infection and the development of POTS in patients who previously didn’t experience dysautonomia. Research has shown that the emergence of dysautonomia in long COVID patients is not associated with the severity of the original COVID-19 infection.
What is POTS?
Postural orthostatic tachycardia syndrome is a form of dysautonomia. People who have POTS will experience a marked increase in their heart rate whenever they stand up. Normally, the ANS balances heart rate and blood pressure regardless of your body’s positioning. If you have POTS, however, the ANS can’t perform this important function.
Imagine standing up. When you do, gravity pulls blood to the lower part of your body. Your ANS attempts to compensate for this by increasing your heart rate to increase blood flow to your heart and brain. Your nervous system will return to normal functioning once your brain has received sufficient blood and oxygen.
This doesn’t happen with people who have POTS. When they stand, the process of increasing blood flow to the brain doesn’t work as it should. The longer they stand, the more blood will pool in the lower half of their body. Prolonged standing, like waiting in line at the grocery store, may cause hypotension (a drop in blood pressure) or hypertension (an increase in blood pressure). This then can cause dizziness, lightheadedness, fainting, brain fog, heart palpitations or chest pain, shakiness, and shortness of breath.
Frustratingly, many people initially seeking care for these unexplained symptoms are incorrectly diagnosed with anxiety, causing unnecessary delays in treatment. For those with long COVID, this often feels like yet another obstacle to overcome—another invisible illness we must convince doctors to believe in.
Long-haulers experiencing symptoms of POTS should address their concerns with their primary care doctors. This is particularly important given that upwards of 14 percent of those infected by COVID-19 develop POTS, while 30 percent of long-haulers meet the criteria.
How is POTS diagnosed and treated?
The symptoms of POTS may resemble a variety of other medical conditions, which can complicate diagnosing. When you consult with a physician about these symptoms, the doctor will likely perform a physical exam and order bloodwork to determine what, if any, other factors may be causing your symptoms. A diagnosis of POTS is typically made by using a standing or tilt-table test.
If you’re diagnosed with POTS, your doctor will discuss treatment options with you. There are many self-care strategies you can easily implement at home. Examples include:
- Increase your salt intake (e.g., your doctor may encourage you to take a salt pill).
- Drink 2-3 liters of water, milk, or electrolyte drinks daily.
- Use natural remedies when nauseous (e.g., ginger, peppermint).
- Briefly tighten and relax your leg muscles several times before standing.
- Maintain an even temperature and don’t become overheated.
- Exercise several times weekly.
- Consider dietary changes (e.g., an antihistamine diet).
- Avoid prolonged standing and bending over whenever possible.
- Educate yourself about your triggers.
Finally, remember that POTS-related symptoms can sometimes be severe or even disabling. Because of this, you have rights under the Americans with Disabilities Act (ADA). Schools and workplaces must make reasonable accommodations to best support your unique needs. For more information, click here.
References
Chadda, K., Blakely, E., et al. (2022). Long COVID-19 and Postural Orthostatic Tachycardia Syndrome- Is Dysautonomia to Be Blamed? Front. Cardiovasc. Med., Volume 9. https://doi.org/10.3389/fcvm.2022.860198
Ormiston, C. K., Świątkiewicz, I., & Taub, P. R. (2022). Postural orthostatic tachycardia syndrome as a sequela of COVID-19. Heart rhythm, 19(11), 1880–1889. Advance online publication. https://doi.org/10.1016/j.hrthm.2022.07.014




