Post-Traumatic Stress Disorder
The Crisis in Veterans' Mental Health and New Solutions
Veteran suicides increase 10-fold from 2006 to 2020.
Posted November 10, 2023 Reviewed by Davia Sills
Key points
- Veterans suffer from high rates of mental health conditions, including PTSD, depression, and substance use.
- Suicides among veterans increased 10-fold from 2006 to 2020.
- New treatment strategies are desperately needed.
- Addressing mental and metabolic health simultaneously may lead to better outcomes.
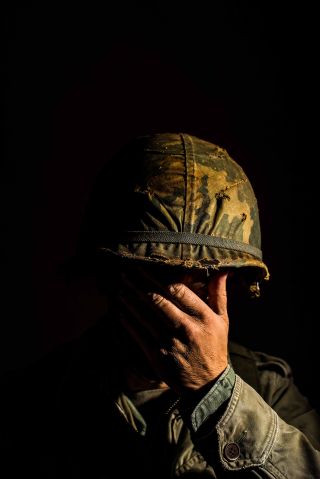
Every year on Veterans Day, we celebrate the brave individuals who have served our country. The mental health challenges that veterans face are both unique and profound. As they transition from service to civilian life, many carry the weight of experiences that significantly impact their well-being. Conventional treatment approaches for conditions such as PTSD, anxiety, depression, and substance abuse are invaluable, yet some veterans continue to struggle with symptoms.
A recent research study published in JAMA Neurology has unearthed a deeply troubling trend: a greater than 10-fold increase in suicide rates among U.S. veterans from 2006 to 2020. Clearly, our current treatment strategies are failing far too many veterans. This is where innovative perspectives, such as the brain energy theory of mental illness, offer fresh hope and understanding.
The brain energy theory, as outlined in this post, posits that mental health conditions are intricately linked with the brain's energy dynamics. A brain with balanced and optimal energy is crucial for mental wellness. For veterans, whose brains are often taxed by the rigors of service and the scars of trauma, ensuring adequate brain energy could be particularly transformative.
Brain energy is, in essence, the currency that powers every thought, emotion, and reaction. This energy stems from the complex interplay of nutrients, hormones, neurotransmitters, and mitochondrial function. For veterans, exposure to stressful environments, trauma, sleep disruption, and physical exertion can lead to a mismatch in energy supply and demand within the brain, potentially exacerbating mental health symptoms.
Research has demonstrated that PTSD, for example, is not just a manifestation of psychological distress but may also be linked to altered metabolism. This can affect the way the brain processes information and responds to stress. By targeting these metabolic processes, we might be able to offer veterans more effective interventions.
How, then, can the brain energy theory guide novel treatment strategies?
- Nutritional Interventions: Tailored nutritional counseling aimed at optimizing brain energy production can be a powerful addition to veterans' treatment plans.
- Exercise and Stress Reduction: Interventions such as targeted exercise regimens may not only enhance overall energy but also improve brain plasticity, resilience, and the regulation of stress hormones. Mind-body practices like yoga and meditation could further aid in rebalancing the brain's energy utilization and emotion regulation mechanisms.
- Specialized Brain Energy Interventions: One promising area is the exploration of supplements, medications, and even light therapy that specifically support mitochondrial function and, consequently, brain energy. While still in the early stages of research, these interventions may offer relief for veterans whose mental health symptoms have been resistant to other treatments. One example is the application of red or near-infrared light to the scalp (transcranial photobiomodulation). In a pilot trial, this intervention was found to improve brain metabolism and reduce symptoms of traumatic brain injury and PTSD.
- Enhanced Psychotherapy: Integrating brain energy optimization into behavioral therapies could amplify their effectiveness. By ensuring the brain is energetically equipped to engage with and benefit from therapy, we can enhance learning, neural growth, and the consolidation of therapeutic gains.
- Comprehensive Care Teams: Coordinated care teams can ensure that veterans receive holistic support, addressing both mental and metabolic health.
The journey toward healing and mental wellness for veterans is both a collective and individual endeavor. By harnessing the principles of brain energy, we can open new avenues for treatment that honor the complexity of the brain and the diversity of experiences among veterans. With continued research and clinical application, this perspective holds the promise of not only alleviating symptoms but also restoring a sense of vitality and hope to those who have served.
As we move forward, it is essential to continue advocating for and investing in research that elucidates the intricate connections between metabolism and mental health. By doing so, we not only pay homage to the sacrifices of our veterans but also elevate our approach to mental health care for all.


