Trauma
Reduce COVID Trauma With Psychological First Aid
Reaching into the psychologist’s toolbox to be proactive in a pandemic.
Posted March 6, 2021 Reviewed by Jessica Schrader
This post was written by Adam R. Klyczek, a member of the Hospital, Healthcare & Addiction Workers, Patients and Families working group of the COVID Psychology Task Force (established by 14 divisions of the American Psychological Association), which sponsors this blog.
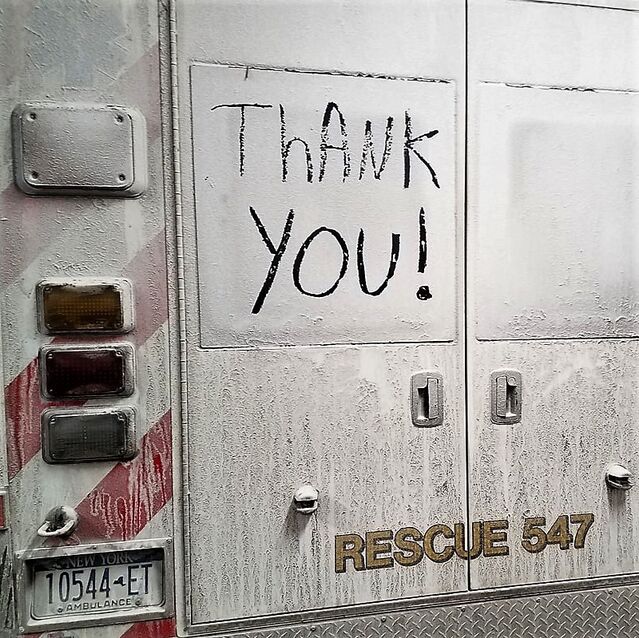
The radio crackles into life as dispatch barks out, “86-year-old male, not conscious, not breathing, repeating for …” The medics jump with a surge of adrenaline and sirens speed toward the scene. Upon arrival, a young woman is giving CPR to her father. Training and muscle memory set in as the medics attempt resuscitation. In an excited frenzy of overlapping orders, protocols, cardiac algorithms, and complex procedures, the patient is loaded into the ambulance and hauled away, leaving nothing but diesel fumes and a wailing siren in the distance.
The distraught daughter stands in the driveway. She cannot go to the hospital due to local restrictions regarding the COVID-19 outbreaks. That is the last time she will see her father.
Psychological First Aid
Psychological First Aid (PFA) may likely produce thoughts of disaster relief workers tending to panic-stricken survivors amid the aftermath of an earthquake or hurricane. That is the genesis of the conceptual intervention, around mid-20th century (Tyhurst, 1951). Recall the cardiac arrest story above; today, particularly during this unprecedented pandemic, the underutilization of this simple tool has been overlooked. The American Psychological Association describes PFA as:
“an initial disaster response intervention with the goal to promote safety, stabilize survivors of disasters and connect individuals to help and resources. PFA is delivered to affected individuals by mental health professionals and other first responders. The purpose of PFA is to assess the immediate concerns and needs of an individual in the aftermath of a disaster, and not to provide on-site therapy.”
Non-professionals can be trained
Psychological First Aid is simple enough to teach to first responders and laypeople, and can also be useful for medical professionals in emergency rooms and intensive care settings, as it does not require training in mental health.
PFA is widely recognized as an effective early intervention, garnishing recommendation within treatment guidelines for posttraumatic stress disorder (PTSD) internationally (Forbes, D., Creamer, M., Bisson, et al., 2010).
However, PFA can and should be employed more broadly. It is clear the ongoing pandemic has exacerbated acute mental health issues, and, when compounded by an extraordinarily stressful event—inherent in any 911 scenario—novel use of existing effective interventions, such as PFA, are called for. The pandemic itself may be viewed as a “disaster,” and so the target population(s) shall necessarily increase, creating a need for well-trained lay practitioners at the scene.
The Upshot & Future Research
Unfortunately, there remains a lack of documented robust data clearly demonstrating PFA’s effectiveness. The American Red Cross commissioned a well-executed systematic review and publication of which PFA was included. The review did confirm the paucity of concrete evidence (Fox, J. H., Burkle, F. M., Bass, J., et al., 2012). Importantly, this does not imply that PFA is ineffective. Consequently, this pandemic has brought with it a call to produce the unrealized data as well as increase the breadth and delivery of PFA to novel target populations.
The Upshots:
- Simple, easy to train, meant for lay personnel and first responders
- Mental health specialists not required
- Cost & Time effective
- Prevents the development of PTSD, adjustment disorder, etc.
-
Broad implementation (first responder training)
-
Possible reduction of mental health inpatient admissions
-
Possible reduction of acute self-harm incidents by trauma survivors
Wrap-up
Let us consider the story at the beginning. The young lady has just experienced a traumatic event compounded by regulations regarding COVID-19, reducing her available resources. Normally, all first responders would have left the scene long ago. On the other hand, should a first responder who is also trained to administer PFA remain, this woman could benefit greatly from the five essential elements of PFA (Hobfoll, S. E., Watson, P., Bell, C. C., el al., 2007):
- Safety
- Calming
- Connectedness
- Self-efficacy
- Hope
These ostensibly commonsensical components may very well allow this woman to begin healing from her trauma much sooner, thus preventing the development of serious and debilitating pathological illness.
COVID-19 has generated far-reaching and unexpected effects. It has created an opportunity to recognize and embrace the potential power of Psychological First Aid in the many crisis situations that arise during the pandemic.
For more information about elements of Psychological First Aid, please consult the APA links below:

Adam is a member of the Military (19) and Trauma (56) Divisions of the American Psychological Association and a doctoral student at McGill University’s Integrated Program in Neuroscience specializing in neuropsychology. His research focuses on neuroplasticity and traumatic brain injury. Adam is a decorated United States Special Operations combat veteran serving two tours as medic to Iraq and Haiti. Adam’s compassionate work while in combat and humanitarian theatres has been internationally recognized. He is active in local rescue, emergency medical services, and fire departments. Additionally, Adam serves on SUNY North Country Community College’s faculty within the Science Department. Contact: AdamKlyczek@gmail.com
References
Forbes, D., Creamer, M., Bisson, J. I., Cohen, J. A., Crow, B. E., Foa, E. B., . . . Ursano, R. J. (2010). A guide to guidelines for the treatment of PTSD and related conditions. Journal of Traumatic Stress, 23(5), 537-552. doi:10.1002/jts.20565
Fox, J. H., Burkle, F. M., Bass, J., Pia, F. A., Epstein, J. L., & Markenson, D. (2012). The Effectiveness of Psychological First Aid as a Disaster Intervention Tool: Research Analysis of Peer-Reviewed Literature From 1990-2010. Disaster Medicine and Public Health Preparedness, 6(3), 247-252. doi:10.1001/dmp.2012.39
Hobfoll, S. E., Watson, P., Bell, C. C., Bryant, R. A., Brymer, M. J., Friedman, M. J., . . . Ursano, R. J. (2007). Five Essential Elements of Immediate and Mid–Term Mass Trauma Intervention: Empirical Evidence. Psychiatry: Interpersonal and Biological Processes, 70(4), 283-315. doi:10.1521/psyc.2007.70.4.283
Tyhurst, J. S. (1951). Individual Reactions to Community Disaster. American Journal of Psychiatry, 107(10), 764-769. doi:10.1176/ajp.107.10.764




