Health
The Patient Safety Risk Model
A strategic data-driven behavioural risk management framework for healthcare.
Posted October 9, 2024 Reviewed by Lybi Ma
Key points
- Preventable mistakes during medical treatment claims hundreds of thousands lives yearly.
- There is an urgent need for more proactive approaches to risk management in the health care system.
- The patient safety risk model predicts safety risks based on doctors' capabilities and performance.
- The patient safety risk matrix identifies risk profiles to identify those at high risk of making mistakes.
Last year, I faced a harrowing experience that would change my perspective on healthcare forever. What began as an emergency surgery to combat a flesh-eating bacteria quickly turned into a nightmare. While the initial procedure went well, a critical oversight nearly cost me my life. Due to negligence, an artery was left unclosed, and I almost bled out that same evening. But looking into it, it seems this isn’t an isolated incidence. In the U.S. alone, medical errors claim around 300,000 lives annually, making it the third leading cause of death. Globally, even in high-income European countries, approximately 1 in 10 patients suffers harm while receiving hospital care. These sobering statistics underscore a grim reality: our healthcare systems can sometimes harm those they aim to help.
This brush with death sparked a burning question: How can we more effectively manage patient safety risks by focusing on healthcare providers themselves? What if we could predict and prevent these errors before they occur? The patient safety risk model is a framework designed to revolutionize how we approach safety in healthcare.
The Patient Safety Risk Model
At its core, the patient safety risk model is a strategic framework that assesses patient safety risks through the lens of healthcare professionals' capabilities and performance. Unlike traditional approaches that focus solely on protocols and systems, this model places healthcare providers at the center of risk management strategies. This dual focus allows us to assess whether healthcare providers possess the skills, knowledge, and psychological readiness to deliver high-quality care under stressful conditions.
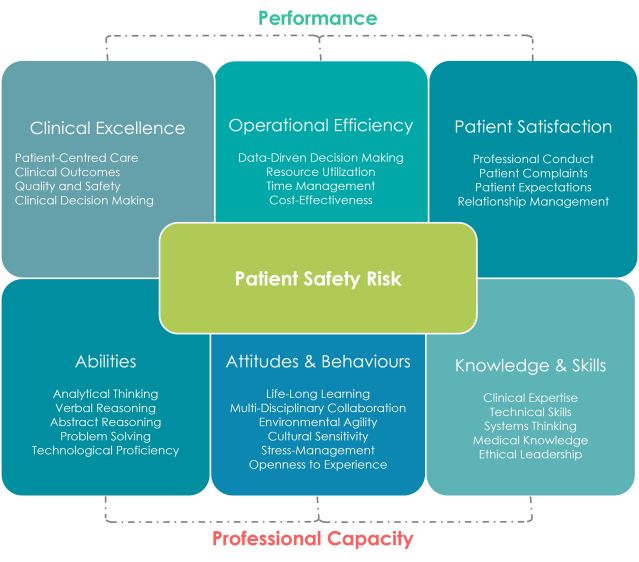
Think of it like this: It’s not enough for a surgeon to know how to perform a technically challenging procedure. They must also have the cognitive bandwidth, emotional resilience, and the right collaborative behaviors to perform consistently well under pressure. The patient safety risk model breaks this down:
- Professional Capacity: It refers to the qualities that enable a healthcare provider to deliver safe, high-quality care. It's not just about what a healthcare professional knows—it's about who they are and how they approach their work. It encompasses cognitive abilities, technical skills, and behaviors like stress management and openness to collaboration.
- Performance: It refers to the practical application of their capacities to provide high-quality care. It’s a function of their clinical decision-making, operational efficiency, and patient satisfaction.
By examining the interplay between these two factors, we can identify potential misalignments that could lead to patient safety risks.
The Patient Safety Risk Matrix: A Visual Tool for Behavioural Risk Management
To bring this model to life, we developed the patient safety risk matrix, a simple yet powerful tool that categorizes healthcare providers into nine risk profiles based on two key dimensions: capacity and performance. By placing doctors on a spectrum, we can identify those at the highest risk for making safety violations but also understand the likelihood of them making mistakes and the potential impact thereof. This allows for more targeted interventions to help them mitigate risks and grow as professionals.
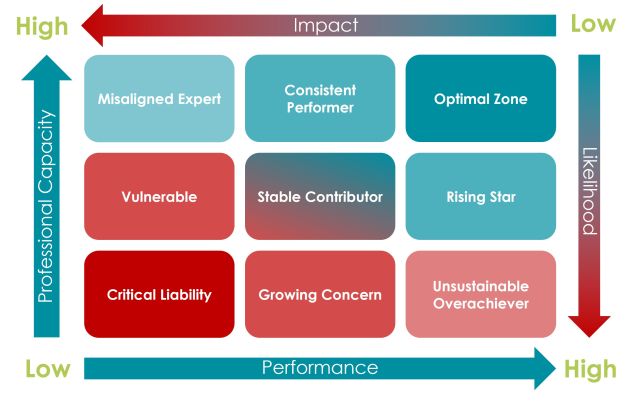
- Critical Liability (Low Capacity, Low Performance): These professionals pose the highest risk to patient safety, lacking essential skills and exhibiting poor performance, necessitating immediate intervention.
- Growing Concern (Low Capacity, Medium Performance): Individuals in this group perform at an average level but have low capacity, presenting a significant risk of performance decline in high-pressure situations.
- Unsustainable Overachiever (Low Capacity, High Performance): This profile includes individuals who are currently performing well despite low capacity, indicating potential burnout or risk of failure under stress.
- Vulnerable (Medium Capacity, Low Performance): These professionals demonstrate average capacity but are underperforming, suggesting they may be hindered by systemic or personal barriers.
- Stable Contributor (Medium Capacity, Medium Performance): Representing the baseline, these professionals maintain a consistent level of performance and capacity but have room for improvement.
- Emerging Talent (Medium Capacity, High Performance): These individuals deliver high performance despite only average capacity, posing a risk of burnout if their skills aren't developed further.
- Misaligned Expert (High Capacity, Low Performance): This category comprises highly skilled professionals whose performance is lacking due to factors like burnout or systemic barriers, posing a significant risk despite their capabilities.
- Consistent Performer (High Capacity, Medium Performance): These healthcare professionals show high capacity and reliable performance, but there’s potential for growth to reach optimal performance levels.
- Optimal Zone (High Capacity, High Performance): The ideal profile represents professionals who consistently excel in both capacity and performance, posing the lowest risk to patient safety and capable of handling complex situations effectively.
Moreover, the matrix allows healthcare organizations to assess not just individual professionals, but also departments or specialties as a whole. Are certain departments clustering in high-risk categories? Are some specialties producing more optimal zone performers than others? These insights can guide systemic interventions and policy changes.
Practical Implications
The power of this matrix lies not just in its ability to categorize, but in how it guides targeted interventions and resource allocation. For instance:
- High-Risk Categories (Critical Liability, Vulnerable, Misaligned Expert): Require immediate and intensive interventions to mitigate patient safety risks.
- Medium-Risk Categories (Growing Concern, Stable Contributor, Consistent Performer): Need ongoing support and development to either maintain their current level or progress to lower-risk categories.
- Low-Risk Categories (Unsustainable Overachiever, Emerging Talent, Optimal Zone): Require strategies to sustain their high performance and prevent burnout or decline.
It can also help inform more strategic interventions, like:
- Personalized Professional Development: Hospitals can tailor training programs based on individual risk profiles, making more efficient use of resources.
- Predictive Risk Management: By regularly assessing medical staff and tracking their movement across the matrix, potential safety incidents can be predicted and prevented.
- Enhanced Recruitment and Onboarding: The model can inform hiring decisions and shape onboarding processes to build a safer workforce from day one.
- Cultural Transformation: It shifts the focus from blame to development, promoting a growth mindset and open discussions about capacity and performance.
A Call to Action: Embracing Data-Driven Patient Safety
With the patient safety risk model, we have a data-driven, proactive approach that empowers healthcare leaders to address the human factors driving errors, rather than simply adding more checklists. Together, we can redefine patient safety—not as a byproduct of flawless systems, but as the outcome of capable, supported, and empowered healthcare professionals.
References
Batt, A., Williams, B., Rich, J., & Tavares, W. (2021). A six-step model for developing competency frameworks in the healthcare professions. Frontiers in medicine, 8, 789828.
Cooper, J. B., Gaba, D. M., Liang, B., Woods, D., & Blum, L. N. (2000). The National Patient Safety Foundation agenda for research and development in patient safety. MedGenMed: Medscape general medicine, 2(3), E38.
de Heer, M. H., Driessen, E. W., Teunissen, P. W., & Scheele, F. (2024). Lessons learned spanning 17 years of experience with three consecutive nationwide competency based medical education training plans. Frontiers in medicine, 11, 1339857.
Donabedian, A. (2005). Evaluating the quality of medical care. The Milbank Quarterly, 83(4), 691–729. https://doi.org/10.1111/j.1468-0009.2005.00397.x
Epstein, R. M., & Hundert, E. M. (2002). Defining and assessing professional competence. JAMA, 287(2), 226–235. https://doi.org/10.1001/jama.287.2.226
Gaba, D. M. (2000). Structural and organizational issues in patient safety: a comparison of health care to other high-hazard industries. California Management Review, 43(1), 83-102.
Kaplan, R. S., & Mikes, A. (2012). Managing risks: A new framework. Harvard Business Review, 90(6), 48–60.
Keijser, W. A., Handgraaf, H. J., Isfordink, L. M., Janmaat, V. T., Vergroesen, P. P. A., Verkade, J. M., ... & Wilderom, C. P. (2019). Development of a national medical leadership competency framework: the Dutch approach. BMC medical education, 19, 1-19.
Leape, L. L., & Berwick, D. M. (2005). Five years after To Err is Human: What have we learned? JAMA, 293(19), 2384–2390. https://doi.org/10.1001/jama.293.19.2384
Lepre, B., Palermo, C., Mansfield, K. J., & Beck, E. J. (2021). Stakeholder engagement in competency framework development in health professions: a systematic review. Frontiers in medicine, 8, 759848.
Makary, M. A., & Daniel, M. (2016). Medical error—the third leading cause of death in the US. BMJ, 353, i2139. https://doi.org/10.1136/bmj.i2139
Maslach, C., & Leiter, M. P. (2016). Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry, 15(2), 103–111. https://doi.org/10.1002/wps.20311
Reason, J. (2000). Human error: Models and management. BMJ, 320(7237), 768–770. https://doi.org/10.1136/bmj.320.7237.768
Stander, F. W., & Van Zyl, L. E. (2019). The talent development centre as an integrated positive psychological leadership development and talent analytics framework. Positive psychological intervention design and protocols for multi-cultural contexts, 33-56.
van der Aa, J. E., Aabakke, A. J., Ristorp Andersen, B., Settnes, A., Hornnes, P., Teunissen, P. W., ... & Scheele, F. (2020). From prescription to guidance: a European framework for generic competencies. Advances in Health Sciences Education, 25, 173-187.
van Engen, V., Buljac-Samardzic, M., Baatenburg de Jong, R., Braithwaite, J., Ahaus, K., Den Hollander-Ardon, M., ... & Bonfrer, I. (2024). A decade of change towards Value-Based Health Care at a Dutch University Hospital: a complexity-informed process study. Health Research Policy and Systems, 22(1), 94.
Vincent, C., & Amalberti, R. (2016). Safer healthcare: Strategies for the real world. Springer Open. https://doi.org/10.1007/978-3-319-25559-0
Zouaoui, I., Drolet, M. J., & Briand, C. (2024). Defining generic skills to better support the development of future health professionals: Results from a scoping review. Higher Education Research & Development, 43(2), 503-520.




