Post-Traumatic Stress Disorder
New Study Shows Brain Change After Psychological Trauma
Research on important findings in earthquake survivors with and without PTSD.
Posted December 5, 2018 Reviewed by Davia Sills
"The drama and the trauma of the relationship you have when you're 16 can mirror the one you have when you're 26. Life repeats itself." —Taylor Swift
Post-traumatic stress disorder (PTSD) is a relatively common condition, affecting nearly 7 percent of people over the course of a lifetime, and over 3.5 percent of people in any given year, according to the NIMH from National Comorbidity Survey data.
Other estimates suggest even higher rates, more so in at-risk groups. PTSD is more than two times higher in women than men, and it is associated with higher suicide rates.
Fifty to 70 percent of U.S. citizens are expected to experience major trauma in a lifetime, and the estimated costs resulting from trauma amount to over $40 billion a year. The burden of PTSD is great in terms of personal suffering, and the impact on family, community, and society from psychosocial and economic perspectives.
What is PTSD?
PTSD is characterized by exposure to a traumatic event, or traumatic events, and may come on shortly after trauma or at a future time. PTSD may be relatively short-lived, or it may be long-lasting, becoming chronic.
PTSD symptoms include a blend of re-living and re-experiencing the trauma—for example via intrusive thoughts, nightmares, or repetitive behaviors (even repeating traumatic relationship patterns)—negative changes in emotions and thinking, for example depressed mood and difficulty with clarity of thought or memory; dissociative symptoms, such as detachment or emotional numbing; avoidance of reminders and thoughts of trauma, which may severely limit one’s choices or keep one from leaving the home; and hyperarousal symptoms, like anxiety, being constantly on edge, or being fearful, rageful, and generally on high alert at all times.
PTSD can only be diagnosed if more than four weeks have passed since a traumatic event; prior to that point, most reactions are considered normal, but if severe may verge diagnostically into Acute Stress Disorder. PTSD, early on in life especially, can lead to complex PTSD (cPTSD), with effects on the development of personality and identity, generally resulting from abuse and neglect as a child.
PTSD and the stress-response system
In general, PTSD represents an exaggerated and persistent reaction to fear in which the two branches of the autonomic nervous system, which regulates the body’s balance between activation and resting, are off-kilter. Normally, the activating branch, the sympathetic nervous system, jumps into action when there is a threat, diverting resources to fight-flight systems... and then things go back to a poised, calmly ready state.
For example, blood flow to the muscles increases, the heart works harder, we become mentally far more alert and sometimes flooded with fear, and we are ready to do what is necessary to survive. When the crisis passes, the parasympathetic system kicks in, and blood flow resumes a normal pattern, the body relaxes, and we may need to use the restroom. Our emotions and thinking settle back down, and we may even at that point need to fuel up before “crashing.”
In PTSD, the activation in a basic sense appears to persist, almost like a computer glitch, and the sympathetic system gets stuck in higher gear, crudely similar to a car running at high RPMs for too long. When this happens, these immediate action systems adapt to chronic usage, leading to ongoing burned-out stress, and negative effects on health and quality of life.
The parasympathetic nervous system is not able to properly cool things down, and either is offline when needed—and we may turn to chemical means to settle ourselves down—or it kicks in when we don’t want it to, causing emotional detachment, fatigue, and a variety of symptoms related to imbalances throughout our systems.
We are not talking about healthy grief or growth after trauma here, though that is an important part of the story and one I personally treasure, but rather prolonged suffering, which serves no additional purpose. It's fine to make lemons out of lemonade if all there is are lemons, but not when there is a fruit stand right next door which we can't seem to get to no matter how hard we try.
It's truly wonderful to glean wisdom from adversity, but it doesn't make sense to seek out adversity in order to become wise.
The brain on PTSD
Given how diverse PTSD is, as is the case with all disorders involving the brain, we don’t have a detailed understanding of what actually happens to cause different kinds of PTSD at different time points. To date, most research has looked at a mixed group of patients with mostly chronic PTSD, with a variety of changes throughout the brain.
The areas of the brain identified to be different in PTSD include the hippocampus, which deals with our memory and sense of self; the amygdala, a main emotion center of the brain emotional systems (limbic system) and a key player in the brain’s state at rest; and the anterior cingulate cortex, which is a key hub in networks for emotion and thought, learning, conflict-resolution, and, notably, top-down control of the limbic system via direct connections with the amygdala.
These brain areas are involved in altered network activity for people who suffer from PTSD, with changes seen in the brain’s resting “default mode network” and the difference in what people with PTSD look for in the environment, in the “salience network.”
Various studies of chronic PTSD have shown conflicting brain anatomical, functional, and metabolic findings in some of the same brain areas, for reasons which are not yet understood.
PTSD, psychoradiology, and earthquakes
Given the few studies of early PTSD and the importance of understanding just what is happening to the brain after a traumatic event, researchers from China and England measured the brain activity of survivors of the 2008 Sichuan earthquake with and without PTSD within seven to 15 months [N.B. of personal significance for me, as I trained mental health responders in China via teleconference right after that earthquake].
After excluding those with other disorders, medication use, prior trauma, head injury, and additional factors which would reduce the statistical power of the study, they had 78 subjects with PTSD and 71 without who were well matched.
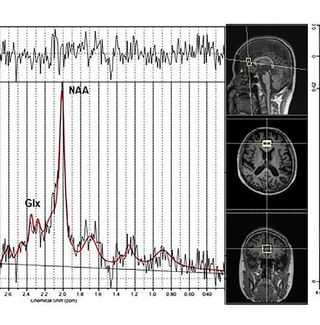
Researchers used “proton magnetic resonance spectroscopy” (H-MRS) to gauge not only the volume of the amygdala (amygdalae, actually, or amygdalas, because there is one on each side), but also metabolic activity in the anterior cingulate cortex (cortices, or cortexes) using spectroscopy, which allows us to infer what molecules are present from analyzing the distribution of different atomic weights in a given sample. Studying metabolic activity to reflect mental activity has been called “psychoradiology,” a developing field as researcher map out which markers mean what, how to measure them, and so forth.
In this study, researchers measured N-acetyl aspartate (NAA), considered to be an indicator of neuron damage or health; creatine (Cr), a general marker of brain activity; glutamate and glutamine (Glx), excitatory neurotransmitters; choline (Cho), reflecting cell density; and Myo-inositol (mI), an indicator related to glial cells, which work in tandem with neurons in supportive and perhaps more direct ways in making up the structure of the brain and allowing our brains to function.
Their findings, while preliminary, are fascinating. They found that NAA concentration in the anterior cingulate was increased in PTSD, higher earlier on and less elevated (but still above non-PTSD) as the months passed. Previous studies of chronic PTSD lean toward lower-than-average NAA, suggesting that NAA is elevated in the early response to trauma in those with PTSD, and an as-yet-unexamined process takes place over time, and NAA drops.
As NAA is higher in other psychiatric conditions and becomes decreased over time (e.g., in depression, schizophrenia, social anxiety disorder), something important is reflected in NAA activity, hypothesized by researchers to be related to increased emotional processing. Both amygdalae were decreased in size, a finding mirroring many, but not all, previous studies. Stress has been shown to reduce amygdala size, but exactly how this happens isn’t clear, especially in the short term.
Metabolic activity was different in the left versus right amygdalae, with high Cr in the left side and high mI in the right. While it is not possible to say what it means, study authors suggest that these differences may be related to the brain’s protective reactions to injury and/or because of glial cells, which are thought to respond to injury by increasing in number and activity.
It isn’t surprising that there are differences between right and left amygdalae, because while similar in function, the different sides of the brain do not have exactly the same functions, associated with differences in amygdala response to trauma and also suggested by prior research.
Where are we in understanding and using knowledge of PTSD neuroscience?
This research is noteworthy for a few reasons. First of all, a picture of PTSD brain changes over time starts to come into focus. The prime example of this is in the finding that NAA is higher right after a traumatic experience leading to PTSD and then tapers off over time, a finding consistent with low NAA levels in long-standing PTSD. The current study allows us to connect the dots between early and later PTSD.
The NAA changes are found in other disorders, pointing to an avenue for further research to understand how chronic mental illness unfolds over time. For example, while NAA level alone may not be a specific way to diagnose PTSD, because it is common in other conditions, NAA level over time may be a way to gauge the progress of care, as could measuring changes in brain volume for conditions where treatment returns the brain to a more normal state.
The other markers are important, because they may end up being helpful stepping-stones along the path to figuring out what short- and long-term trauma and stress do to the brain. In addition, though this is a stretch, the data from this and other research might be used to construct a diagnostic tool specific for PTSD, which could help to tell PTSD apart from other conditions early on in treatment and, again, to track clinical response as well as point the way to new therapies.
More broadly, H-MRS and related psychoradiological tools will continue to transform our understanding of the “mindbrain,”1 the holistic union of biological and psychological processes which make up our psyches, envisioned early on by Sigmund Freud in his Project for a Scientific Psychology (1895).
We are gradually developing and using new methods to catch deeper and deeper glimpses of what is going on which makes us who and what we are, in sickness and in wellness. We are coming to grasp that psychological trauma physically impacts the brain immediately following an injury, and over time.
Being able to analyze metabolic activity and understand what it means is a key part of the puzzle, along with looking at changes in brain volume and activity based on blood flow. All of these approaches can help inform our understanding of altered brain networks, a crucial conceptual tool for seeing the brain as a dynamic, measurable system; as a framework for molding brain activity back to a non-PTSD state (e.g., using targeted neuromodulation, like transcranial magnetic stimulation, or TMS, and other therapeutics); and to help understand how to support and establish resilience.
It will be important to see how the approaches used in this work develop, and how they are applied to a broader group of people. Understanding the brain processes which underlie PTSD will help us to understand how trauma repeats itself, especially with early trauma, which leaves a stronger imprint on development and personality, and how to find healthier alternatives to automatic, often helpless repetition, which persists in spite of intellectual understanding.
References
1. As Mark Blechner, PhD calls it in his work on the neuroscience of dreaming in The Mindbrain and Dreams: An Exploration of Dreaming, Thinking, and Artistic Creation
Xiaorui S, Chunchao X, Wang W, Huaiqiang S, Qiaoyue T, Simin Z, Lingjiang L, Kemp G, Qiang Y and Qiyong G. Abnormal metabolite concentrations and amygdala volume in patients with
recent-onset posttraumatic stress disorder. Journal of Affective Disorders, online 11 August 2018.




