Stress
Beyond Stress and Burnout: What Is Psychoneuroimmunology?
Taking the stress out of stress.
Posted February 2, 2022 Reviewed by Davia Sills
Key points
- Just about everyone faces the effects of burnout and stress.
- Burnout is not exclusive to work; it can occur in any setting.
- Psychoneuroimmunology (PNI) considers the effects of neurotransmitters, hormones, and the immune system on thoughts, feelings, and behaviors.
- PNI factors underlie stress and burnout, so understanding PNI can help address the detrimental effects of stress, boosting therapeutic results.
It seems that you can’t read any newspaper or magazine today without stress and burnout being a main topic of coverage. With the stressors of COVID, politics, job turnover, family obligations, violence, economic concerns, worldwide instability, and just trying to take care of yourself—well, it’s no surprise that we are burned out. A frequently reported study by Indeed.com, as provided in Forbes, found that 52 percent of workers reported being burned out, an increase of 67 percent since the COVID pandemic (2021). And if you happen to be a leader in a health care setting, the burnout rate goes up to 73 percent before COVID (MGMA, 2018).
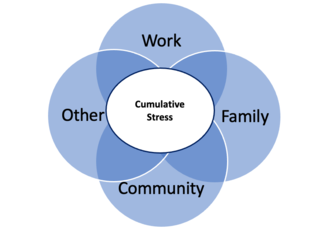
Keep in mind that these rates only discuss burnout that is work-related. However, burnout is not exclusive to work; it's a stress-induced disorder. As a result, we can have stress and burnout in any area of our lives, and the effects are cumulative.
I have been a hospital CEO for 20 years and a Doctor of Psychology, so I have seen first-hand the dramatic impact that stress and burnout have on others, and I am certainly all too familiar with the terrible toll it has taken on me personally. But there is certainly hope, as burnout can be effectively dealt with. My goals for this page are to help readers to:
- Understand their unique stress and burnout symptoms better.
- Prepare actions and plans to deal with them.
- Implement those plans successfully.
To achieve this, I will use a theoretical framework grounded in psychoneuroimmunological (PNI) concepts provided in easy-to-understand formats. By using this framework, therapists and patients (and anyone) can better grasp burnout and craft more effective strategies to reduce the underlying stress.
What is psychoneuroimmunology (PNI)?
So, to start, as psychoneuroimmunology is quite a haughty name, it is important to discuss what it actually is. In its simplest form, PNI studies the interactions of cognitive processes, emotions, and behaviors (psycho) with the influence of neurotransmitters and brain structures (neuro) and inflammatory processes led by pro-inflammatory proteins called cytokines (immuno). There is one more important factor to consider—the endocrine system with the involvement of select hormones. These are somewhat loosely included in the neuro portion of psychoneuroimmunology from the context that hormonal pathways stem from activation in the hypothalamus-pituitary-adrenal (HPA) axis.
From one context, these interactive factors embodied in PNI largely underlie the stress-reactive process, commonly referred to as fight-or-flight in the popular media. Importantly, the fight-or-flight concept is quite limited in scope and not an entirely accurate way to describe stress reactivity.
When stress occurs, your body releases these neurotransmitters, hormones, and cytokines. This is quite beneficial if the stress is acute in nature or results from an emergent threat, requiring immediate action to save your life; however, when stress becomes chronic and uncontrolled, these molecules cause considerable psychophysiological damage.
Chronic stress has been reported as permissive in diseases, including chronic inflammatory diseases, autoimmune disorders, cancer, cardiovascular diseases, diabetes, endocrinological diseases, irritable bowel syndrome, acute and chronic viral infections, sepsis, and asthma, to name a few (Bonaz et al., 2018; Straub & Cutolo, 2017; Streeter et al., 2012). Additionally, a chronically activated immune system and active cytokine presence interfere with electro neurochemistry, leading to a range of psychological disorders, dementia, post-traumatic stress sequelae, fatigue, poor sleep quality, depression, irritability, cognitive difficulties in attention and memory, and anxiety (Moraes et al., 2018; Rodriguez et al., 2018; Straub & Cutolo, 2017). Finally, psychosomatic issues, major depression, social phobia, panic disorder, generalized anxiety, obsessive-compulsive disorder, susceptibility to infectious diseases, and cardiovascular disorders have been found to be associated with a dysfunctional HPA axis (Streeter et al., 2012; Verma et al., 2011).
In sum
PNI describes a complex but coordinated psychophysiological process that is at the heart of stress reactions and chronic dysregulation. But most importantly, many of the stress reactions that occur are preventable in nature through well-researched psychological and stress-based mitigation techniques.

The link with PNI and stress management dates back thousands of years in Eastern traditions through cognitive and somatic-based mindfulness practices (Comer, 2020); however, research in this area is quite recent from a Western medical standpoint—but, fortunately, it is growing in leaps and bounds. Regardless of the therapeutic approach practiced, knowing how to incorporate basic PNI concepts into therapeutic assessments and plans can provide a much more informed approach to helping clients to understand and improve mental health conditions and what underlies them.
We have a lot to cover, so get your neurotransmitters, hormones, and cytokines excited and join me as we go forward in learning how to beat burnout.
References
Bonaz, B., Bazin T., & Pellissier, S. (2018). The vagus nerve at the interface of the microbiota-gut-brain axis. Frontiers of Neuroscience, 12, 49. https://doi.org/10.3389/fnins.2018.00049
Comer, W.J. (2020). Mindfulness-based treatments for veterans with post-traumatic stress disorder: A systematic literature review. Doctoral Dissertation. California Southern University, Costa Mesa, CA.
Kelly, J. (2021). Indeed study shows that worker burnout is at frightening high levels: Here's what you need to do now. https://www.forbes.com/sites/jackkelly/2021/04/05/indeed-study-shows-th…
Medical Group Management Association (MGMA). (2018). Guarding against burnout in your practice. https://www.mgma.com/data/data-stories/guarding-against-burnout-in-your…
Moraes, L.J., & Miranda, M.B. (2017). A systematic review of psychoneuroimmunology-based interventions. Psychology, Health, and Medicine, 23(3), 1-8. https://doi.org/10.1080/13548506.2017.1417607
Rodriquez, E. J., Livaudais-Toman, J., Gregorich, S. E., Jackson, J. S., Nápoles, A. M., & Pérez-Stable, E. J. (2018). Relationships between allostatic load, unhealthy behaviors, and depressive disorder in U.S. adults. Preventive Medicine, 110, 9–15. https://doi.org/10.1016/j.ypmed.2018.02.002
Straub, R.H., & Cutolo, M. (2017). Psychoneuroimmunology: Developments in stress research. Wien Med Wochenschr, 168(3), 76-84. https://doi.org/10.1007/s10354-017-0574-2
Streeter, C.C., Gerbarg, P.L., Saper, R.B., Ciraulo, D.A., & Brown, R.P. (2012). Effects of yoga on autonomic nervous system, gamma-aminobutyric acid, and allostasis in epilepsy, depression, and post-traumatic stress disorder. Medical Hypotheses, 78(5):571-9. https://doi.org/10.1016/j.mehy.2012.01.021
Verma, R., Singh-Balhara, Y.P., & Gupta, C.S. (2011). Gender differences in stress response: Role of developmental and biological determinants. Industrial Psychiatry Journal, 20(1), 4-10. https://doi.org/10.4103/0972-6748.98407


