Health
Asian American Elders Report Low Support, Life Satisfaction
Korean American elders may be at particular risk.
Posted February 21, 2022 Reviewed by Kaja Perina

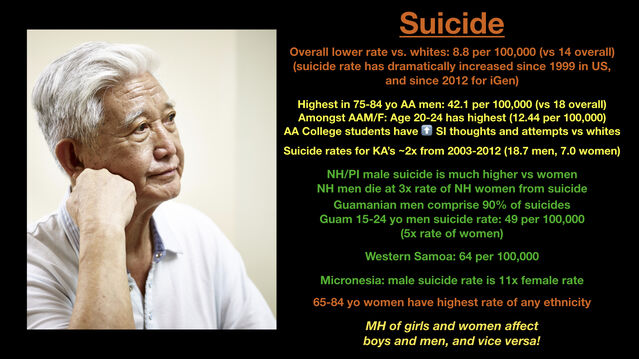
A recently published study in the Journal of the American Board of Family Medicine reports that several groups of Asian American elders reported significantly lower levels of life satisfaction and receiving social and emotional support, compared to aggregated non-Asian American elders. The study was based on California survey data in 2018, so it is unclear what the COVID-19 pandemic and surge in anti-Asian hate has done to these measures. Of significance, previous data indicate older Asian Americans have higher rates of suicide than the general population, and Korean Americans experienced a doubling of suicide rates from 2002-2012.
Asian American elders are at increased risk, and this requires more study and psychosocial intervention.
Epidemiologist Riti Shimkhada of UCLA and colleagues used data from the 2018 California Health Interview Survey, sampling 8,518 individuals age 65 and older. Sample size was significant for comparison for four Asian American subgroups: Chinese, Korean, Filipino, and Vietnamese Groups. In aggregate, only 54% of Asian American elders reported life satisfaction at 7 or above on a scale of 10, as opposed to 80% of non-Asian American elders. Only 56% of Asian American elders reported usually or always receiving social and emotional support, as opposed to 80% of non-Asian American elders. The authors report “[T]here were no significant differences in poverty (under 200% federal poverty level), living alone (1 in household), % married, years lived in United States (10+ years), age, place of residence (urban, rural, suburban) between any of the [65 and older Asian American] subgroups.”
There were differences between Asian American subgroups. “Korean older adults reported significantly lower social/emotional support (30%) compared with Chinese (57%) and Filipino (59%) older adults (P < .05 level).” Korean elders also had the lowest level of life satisfaction at about 40%, compared to Filipino elders at 77%, and Chinese and Vietnamese at about 48% each, but this difference did not rise to statistical significance.
What is unclear is how these numbers translate into actual DSM-5 diagnoses such as depression and anxiety. What is known is that Asian Americans self-report higher levels of distress that do not translate into DSM diagnoses, possibly indicating the presence of cultural syndromes, histories, and other factors that need sensitivity and further research and treatment.
Certainly in my social circles and social media feeds, I’ve seen wide evidence of Asian Americans concerned about their elder parents in terms of health and safety during these difficult times. There has been an active effort to support elders in major cities, through chaperoning and through food and service delivery. How did these additional supports weigh against the increased stresses of COVID and anti-Asian hate? It may take years to know the results. What’s clear is that Asian American elders have specific needs and vulnerabilities that have not been met.
(c) 2022 Ravi Chandra, M.D., D.F.A.P.A.
References
Simkhada R, Tse HW, Ponce N. Life Satisfaction and Social and Emotional Support Among Asian American Older Adults. Journal of the American Board of Family Medicine. Jan-Feb 2022 (35:1), 203-205.
Chandra R. SF Love Dojo Lectures on Asian American Psychology. 2019
Kung A, Hastings KG, Kapphahn KI, Wang EJ, Cullen MR, Ivey SL, Palaniappan LP, Chung S. Cross-national comparisons of increasing suicidal mortality rates for Koreans in the Republic of Korea and Korean Americans in the USA, 2003-2012. Epidemiol Psychiatr Sci. 2018 Feb;27(1):62-73. doi: 10.1017/S2045796016000792. Epub 2016 Nov 10. PMID: 27830639; PMCID: PMC6998889.


