Meditation
The Neuroscience of Mindfulness Meditation and Pain Relief
Mindfulness meditation is proven to reduce pain at a neurobiological level.
Posted November 11, 2015

Over 100 million Americans are impacted by chronic pain, which is the leading cause of disability in the United States. The financial toll of pain is estimated to be $560 to $630 billion annually between the cost of medical expenses and absenteeism.
In 2014, the National Institute of Health (NIH) compiled a report, "Pathways to Prevention: The Role of Opioids in the Treatment of Chronic Pain" to address the silent epidemic caused by the prevalence of chronic pain and the use of highly addictive opioids to treat pain. Ultimately, this report is a call-to-action for more research to find drug-free alternatives for the treatment of pain.
In 1991, doctors wrote 76 million prescriptions for opioids to treat pain. By 2011, this number had almost tripled to 219 million. Unfortunately, according to the NIH report, 40 to 70% of people with chronic pain aren't actually receiving the proper medical treatment for their pain. In cases where opioids are necessary, there is concern by experts about both the over- and under- pharmacological treatment of chronic pain.
A staggering 80% of all opioid prescriptions worldwide are written in the United States. It appears that other countries have found different treatments for chronic pain. What can Americans do to find nonpharmacological treatments for their physical and psychological pain?
Mindfulness Meditation and Nonpharmacological Pain Management
In recent years, a growing body of evidence has found that mindfulness and meditation have the ability to relieve pain by creating structural and functional changes in the brain. I've written a broad range of Psychology Today blog posts on this topic. In this post, I've compiled the latest science-based findings in a retrospective analysis of "The Neuroscience of Mindfulness Meditation and Pain Relief."
Most recently, scientists at Wake Forest Baptist have found new evidence that mindfulness meditation reduces pain more effectively than placebos by activating two specific brain regions associated with self-control, and deactivating the thalamus.
The November 2015 study reports that mindfulness meditation outperforms a placebo in pain reduction. The report was published in the Journal of Neuroscience. These findings are significant because placebo-controlled trials are necessary to demonstrate the efficacy of clinical and pharmacological pain treatments.
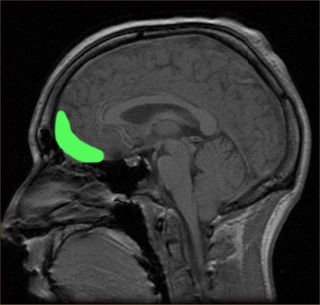
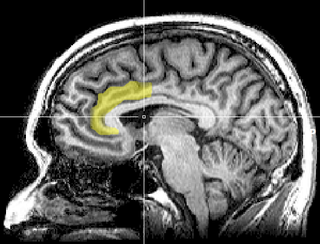
The researchers found that mindfulness meditation reduces pain by activating the orbitofrontal cortex (OFC) and anterior cingulate cortex. According to the researchers, these brain areas are associated with the self-control of pain. Mindfulness meditation also deactivated the thalamus, which acts as a type of gateway to determine which sensory information is allowed to reach higher brain centers.
In a press release, lead author Fadel Zeidan, assistant professor of neurobiology and anatomy at Wake Forest Baptist, described the study,
"While we thought that there would be some overlap in brain regions between meditation and placebo, the findings from this study provide novel and objective evidence that mindfulness meditation reduces pain in a unique fashion. This study is the first to show that mindfulness meditation is mechanistically distinct and produces pain relief above and beyond the analgesic effects seen with either placebo cream or sham meditation."
Orbitofrontal cortex (OFC) in green.Source: Wikimedia Commons/Public Domain
These findings support another study from earlier this year which identified two different brain pathways that contribute to the pain experience and can be self-regulated. The January 2015 Colorado University-Boulder study, “Distinct Brain Systems Mediate the Effects of Nociceptive Input and Self-Regulation on Pain,” was published in the journal PLOS Biology.
Interestingly, a September 2015 study from the University of Illinois at Urbana-Champaign identified that healthy adults who have a larger orbitofrontal cortex (OFC) tend to have less anxiety and are more optimistic. The study, “Optimism and the Brain: Trait Optimism Mediates the Protective Role of the Orbitofrontal Cortex Gray Matter Volume Against Anxiety,” was published in the journal Social, Cognitive and Affective Neuroscience.
Mind-Body Practices Can Help Prevent and Improve Chronic Pain
Chronic pain triggers changes in brain structure that are linked to depression, anxiety, and impaired cognitive function. Brain imaging studies have shown that chronic pain leads to changes in gray matter volume and the integrity of white matter connectivity. Gray matter is home to the neurons in specific brain regions, while white matter creates communication lines between your various brain regions.
In May 2015, Catherine Bushnell, Ph.D., gave a lecture entitled,“Effect of Environment on the Long-Term Consequences of Chronic Pain,” at the American Pain Society's annual meeting in Palm Springs. Bushnell and her colleagues at the NIH are conducting research aimed at discovering non-pharmacological treatments for pain. They've found that chronic pain can be prevented, or reversed, through mind-body practices.
After assessing the impact of brain anatomy on pain reduction, Bushnell concluded that gray matter changes in the insula or internal structures of the cerebral cortex are the most significant players involved in chronic pain.
The researchers used diffusion tensor brain imaging to analyze gray matter volume and the integrity of white matter tracts. Bushnell hypothesizes that increased size and connectivity of the insular cortex is probably the most important brain factor regarding changes in an individual's pain tolerance and thresholds.
Bushnell found that Yoga appears to bulk up gray matter through neurogenesis (the growth of new neurons) and strengthens white matter connectivity through neuroplasticity. "Insula gray matter size correlates with pain tolerance, and increases in insula gray matter can result from ongoing yoga practice," Bushnell said in a press release.
Yoga practitioners have more gray matter than controls in multiple brain regions, including those involved in pain modulation. Other studies have found that regular physical activity is linked to optimizing gray matter volumes and the integrity of your brain's white matter throughout a lifespan.
Conversely, in a series of groundbreaking experiments, Daniela Kaufer, University of California, Berkeley associate professor of integrative biology, and her colleagues discovered that chronic stress and elevated levels of cortisol can disrupt gray matter brain volume and white matter connectivity. In 2014, Kaufer et al. published the study, "Stress and Glucocorticoids Promote Oligodendrogenesis in the Adult Hippocampus," in the journal Molecular Psychiatry.
Could Small Acts of Gratitude and Empathy Help Reduce Pain?
One thing that jumped out at me after reading the new study from Wake Forest this morning was the correlation between mindfulness, pain reduction, and the activation of the anterior cingulate cortex.
Last month, I wrote a Psychology Today blog post, "Small Acts of Generosity and the Neuroscience of Gratitude," based on a study led by Antonio Damasio at USC which found that ratings of gratitude correlated with brain activity in the anterior cingulate cortex.
The October 2015 study, “Neural Correlates of Gratitude,” was published in the journal Frontiers in Psychology. Although it is pure conjecture on my part, and an educated guess, it would seem that loving-kindness meditation and nurturing feelings of gratitude could possibly trigger brain changes that activate the anterior cingulate cortex which is also related to pain reduction.
Along these lines, in 2014 neuroscientists in Italy reported that “social pain” activates the same brain regions as physical pain. The researchers also found that witnessing the social pain of another person activated a similar physical pain response of empathy in most test subjects.
The February 2014 study, “Empathy for Social Exclusion Involves the Sensory-Discriminative Component of Pain: A Within-Subject fMRI Study,” was published in the journal Social Cognitive and Affective Neuroscience. This study also found direct links to the posterior insular cortex (also called the insula).
These findings beg the question: Could the triad of empathy, gratitude, and generosity work together to create an analgesic ripple effect and upward spiral for social and physical pain on a neurobiological level? To my knowledge, there is no research that has studied this specific topic—but I will keep my antennae up for any new research in this field.
Conclusion: Mindfulness Meditation as an Opioid Alternative for Treating Pain
The lethal consequences of opioid addiction have been making headlines in recent weeks. The statistics are alarming. Last week, I wrote a Psychology Today blog post, "Why Are So Many Middle-Aged White Americans Dying Young?" that was inspired by a CDC study which found that drug overdoses now cause more deaths than car crashes, with opioids like OxyContin and other pain medications killing 44 people a day.
Deaths from heroin have quadrupled since 2013 claiming 8,260 lives. Some experts at the CDC are calling this the worst drug overdose epidemic in U.S. history. A July 2014 study, “The Changing Face of Heroin Use in the United States,” concluded, “Although the ‘high’ produced by heroin was described as a significant factor in its selection, it was often used because it was more readily accessible and much less expensive than prescription opioids.”
Mindfulness meditation is not a silver bullet for ending what the NIH called the 'silent epidemic' caused by the prevalence of chronic pain and the use of highly addictive opioids to treat pain. However, mindfulness meditation and other mind-body practices are science-based interventions that have been proven to help people manage both physical and psychological pain.
If you'd like to read more on this topic, check out my Psychology Today blog posts,
- "10 Ways Mindfulness and Meditation Promote Well-Being"
- "Neuroscientists Identify How Mindset Alters Pain Perceptions"
- "Cortisol: Why the Stress Hormone Is Public Enemy No. 1"
- "How Does Yoga Relieve Chronic Pain?"
- "5 Neuroscience Based Ways to Clear Your Mind"
- "Optimism and Anxiety Change the Structure of Your Brain"
- "How Are Human Traits Linked to Specific Brain Connections?"
- "Can Meditation Make Someone More Compassionate?"
- "Mindfulness Training and the Compassionate Brain"
- "The Neuroscience of Social Pain"
- "Is Impaired Neuroplasticity Linked to Chronic Pain?"
- "Chronic Stress Can Damage Brain Structure and Connectivity"
- "The Neurobiology of Grace Under Pressure"
- "Mindfulness: The Power of "Thinking About Your Thinking"
- "The Neuroscience of Savoring Positive Emotions"
- "7 Ways to Create an Upward Spiral of Positive Emotions"
- "Neuroscientists Confirm That Our Loved Ones Become Ourselves"
© 2015 Christopher Bergland. All rights reserved.
Follow me on Twitter @ckbergland for updates on The Athlete's Way blog posts.
The Athlete’s Way ® is a registered trademark of Christopher Bergland.




