Psychopharmacology
The Link Between Payments and Prescribing
A systematic review finds a clear association.
Posted November 30, 2020 Reviewed by Ekua Hagan
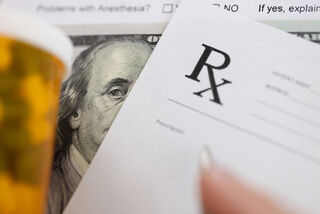
Financial payments from U.S. drugmakers to the nations’ physicians are common. Between 2015 and 2017, according to a study published last year in the British Medical Journal, 67 percent of all U.S. physicians received payment of some kind. Smaller payments are more common, mostly as reimbursement for food and beverages, yet researchers have found it difficult to prove a clear and direct influence on prescribing.
That is no longer the case. In the November 2020 issue of the Annals of Internal Medicine, Aaron P. Mitchell and colleagues in Epidemiology and Biostatistics at Memorial Sloan Kettering Cancer Center, New York City, present overwhelming evidence that the “receipt of financial payments from industry is consistently associated with increased prescribing.” Their systematic review determines also that “industry payments are associated with increased use of lower-value drugs” and that “evidence of a temporal association and dose-responsiveness strongly suggests a causal relationship.”
Of the 36 studies included in the review, themselves comprising 101 analyses, 30 “found only positive associations between industry payments and prescribing in all constituent analyses. Six had mixed results, reporting one or more positive associations and one or more null associations among their analyses.” No study reported only null results.
Each found a “positive association between payments and prescribing in 1 or more of its constituent analyses.” These included several types of prescribing decisions, making it possible to determine, write Dr. Mitchell and colleagues, “that physicians who had received industry payments were more likely to prescribe drugs made by the companies that had paid them than alternatives, had higher prescribing costs, and prescribed a higher proportion of brand-name products over generic alternatives.”
The review, supported by a National Cancer Institute Memorial Sloan Kettering Cancer Center Support Grant, drew without restriction from five databases: MEDLINE (Ovid), Embase, the Cochrane Library (Wiley), Web of Science Core Collection (Clarivate), and EconLit (EBSCO). The design was observational, so some of the studies are flagged as carrying a moderate risk of bias.
From 2013, Mitchell and colleagues note, the Open Payments reporting system created by the Physician Payments Sunshine Act has “made public all financial transfers greater than $10 in value from drug and device manufacturers to U.S. physicians and several other provider groups, including chiropractors and dentists.” That, in turn, has made it possible to review comprehensive data on industry payments and prescribing alongside equally granular data on physicians’ prescribing volumes, including within different drug classes, to determine when consultancy fees, honoraria, and even food and beverage payments have influenced their prescribing.
Of the 36 studies, 25 assessed for a dose-response relationship between payments and prescribing. “All 25 studies found evidence of a dose-response relationship in 1 or more of their primary analyses.”
The review joins a number of recent studies confirming drug-industry influence on various sectors of American medicine, from physician formulary recommendations to clinical research and clinical practice guideline recommendations. Lacking financial data from before the Physician Payments Sunshine Act, previous studies tended to measure influence in nonfinancial terms, including via frequency of office visits by sales reps.
The just-published review confirms that payments are a key factor driving prescribing: “Receiving payments from a drug company” is shown to “lead a physician to prescribe more of that company’s drug in the future.” Second and equally concerning, prescribing may in turn cause payments. “Drug companies may target payments to physicians who are already high prescribers of their drugs. Both mechanisms are plausible.”
Given the authors’ concerns about the diminished quality of care, they note that “payments were associated with a range of adverse prescribing quality measures, such as benzodiazepine prescriptions of longer than 12 weeks' duration and vasodilator prescriptions for patients older than 65 years.”
Concerning prescribing patterns tied to opioids, erectile dysfunction drugs, antipsychotics, and other drugs assessed, the study authors also found evidence of “product hopping”—the promotion of newer products in anticipation of patent expiration on an older one.
The publication is especially timely as Purdue Pharmaceuticals pleaded guilty last week to “paying illegal kickbacks to doctors who prescribed OxyContin and to an electronic health records company, Practice Fusion, for targeting physicians with alerts that were intended to increase opioid prescriptions.” As Katie Benner reported in the New York Times, “Doctors overprescribing OxyContin, along with illicit distribution of the drug, have contributed to the deaths of more than 450,000 Americans since 1999.”
Despite some well-publicized controversy, including proposed rebates for overdoses, “physician opposition … has been an important barrier to reform,” note Dr. Mitchell and colleagues in the Annals of Internal Medicine. “Most physicians have historically believed that receiving industry gifts is appropriate and that this practice should continue.” While “physicians’ opposition to ending financial payments from the drug industry may be rooted in the belief that accepting such payments will not affect their practice,” they add, the opioid epidemic proving a strong case in point, “our findings suggest that this belief is not well-founded.”
Among their concerns: payments may influence physicians’ clinical decision-making and fuel overprescribing by creating a sense of obligation, reciprocity, or openness to influence. “The medical community must change its historical opposition to reform,” Mitchell and colleagues conclude, “and call for an end to such payments.” If they will not do so, then clearly Congress must take action on their behalf.
References
Mitchell Aaron P, Trivedi Niti U, Gennarelli Renee L, et al. (2020). “Are Financial Payments From the Pharmaceutical Industry Associated With Physician Prescribing?: A Systematic Review.” Ann Intern Med. (2020 Nov 24). PMID: 33226858 DOI: 10.7326/M20-5665. Online ahead of print. [Link]




