Suicide
When Is Suicide Acceptable?
Rationality, morality, and cultural relativism.
Posted April 6, 2015 Reviewed by Devon Frye
“When you don’t have any more doors to open, death is a door.” —Vladimir Ceballos
This past fall, Brittany Maynard attracted national attention with the announcement that she intended to end her life by physician-assisted suicide in the face of terminal cancer. At the start of 2014, Maynard was diagnosed with a brain tumor, which quickly advanced despite surgery such that by the spring she was told she would die within the year. With this news, she moved from California to Oregon, one of a handful of states in the U.S. where physician-assisted suicide is legal, and ultimately ended her life by that means, surrounded by family, just a few weeks shy of her 30th birthday on November 1, 2014.
Although increasing numbers of people support the legalization of physician-assisted suicide, Maynard’s case attracted an unusual amount of public debate after she partnered with and became something of a poster child for the organization Compassion & Choices, the largest nonprofit group at the heart of the “death with dignity” movement here in the U.S. With the release of two moving and professionally edited videos (see them here and here), many viewed her story with sympathy and rallied around her “right to die.”
But others argued that she was making the wrong choice. For example, Dr. Ira Byock of the Providence Institute for Human Caring said in an interview that Maynard was being exploited and that she could attain death with dignity and minimal suffering with conventional palliative care (palliative care is a subspecialty branch of medicine that provides end of life and hospice care). Others opined that suicide under any conditions was immoral, with a Vatican official calling Maynard’s decision “absurd” on the grounds that it was “saying no to life.”
These varied reactions to Maynard’s case mirror a national divide over general attitudes about euthanasia, an umbrella term for taking measures to end the life of someone with unbearable suffering associated with an intractable or terminal illness. A recent Gallup Poll reported that 70 percent of Americans answered “yes” to the question, “When a person has a disease that cannot be cured, do you think doctors should be allowed by law to end the patient's life by some painless means if the patient and his family request it?” A smaller 51 percent majority answered “yes” to the question, “When a person has a disease that cannot be cured and is living in severe pain, do you think doctors should or should not be allowed by law to assist the patient to commit suicide if the patient requests it?”
Although both Gallup Poll questions ask about euthanasia in some form, there are some relevant differences. The first question about a doctor “ending a patient’s life by painless means” is technically asking about “active voluntary euthanasia” in which a physician administers a medication that hastens death. The second question asking about a doctor “assisting a patient to commit suicide” refers to “physician-assisted suicide” in which a doctor provides the medication that the patient then self-administers. Interestingly, while the Gallup Poll suggests greater public acceptance of active voluntary euthanasia, only physician-assisted suicide is legal in the U.S.
Beyond the technical differences in the role of a doctor in active voluntary euthanasia and physician-assisted suicide, differences in the wording of the Gallup Poll questions and their implied meaning seem important to public acceptance. As much as there are persistent cultural taboos against suicide in the U.S., the use of that term in the second question might be troubling to some. Just so, pro-euthanasia organizations have shifted away from the terms suicide and even euthanasia (despite its literal meaning “happy death”) in favor of the newer catchphrases “death with dignity” and “right to die.” Increasing public acceptance of euthanasia, therefore, seems to require that its meaning is transformed into something apart from run-of-the-mill suicide. Nonetheless, it remains a subject of intense disagreement.
In order to understand the divide over euthanasia, examining the rationale behind those who support and oppose it seems a sensible place to start. Proponents back the legalization of physician-assisted suicide on the grounds that it promotes self-determination and avoids unnecessary suffering in the setting of advances in medical care, which somewhat ironically can prolong the duration of life at the expense of quality.
Opponents raise questions about the role of depression in decisions to end life and cite slippery-slope arguments, noting that other countries now allow euthanasia for those who lack “mental competency” including children or certain individuals with mental illness. Still others object to euthanasia on purely religious grounds, noting that “only God should decide the time of death.” In fact, religious affiliation is one of the best predictors of whether one supports the legalization of physician-assisted suicide. This is not surprising given that religious beliefs are often linked to moral beliefs dictating concepts of “right” and “wrong.”
Indeed, public acceptance of euthanasia ultimately boils down to a question of morality, where moral values are loosely defined as what is considered to be right or wrong in terms of human behavior. But while morals are often held by individuals as if they’re absolutes, there are in reality subject to considerable cultural relativism—what is acceptable in one culture or subculture is often unacceptable in another. While at first glance suicide might seem to be a nearly universal taboo, the issue of euthanasia in the U.S. illustrates how suicide under certain conditions may take on a different meaning and gain widespread acceptance.
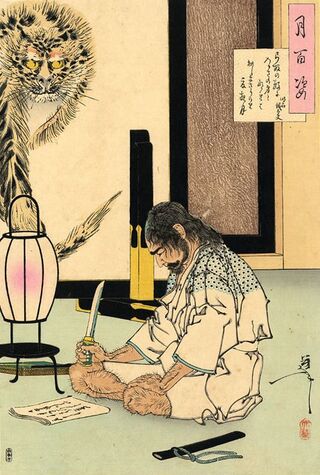
Looking beyond the case of euthanasia in the U.S. further highlights the cultural relativism of suicide. This is something that I’ve recently explored in a paper called “Culturally Sanctioned Suicide: Euthanasia, Seppuku, and Terrorist Martyrdom,”1 where I review the increasing acceptance of euthanasia in developed Western countries along with other examples of culturally sanctioned suicide that many of us in the West find completely foreign.
For example, there’s probably no more iconic form of culturally accepted suicide in history than the Japanese tradition of ritual disembowelment called seppuku or hara-kiri. Yet despite its romanticization in literature and movies, there has never been an equivalent in the West. Likewise, ever since 9/11, considerable effort has been devoted to understanding the kind of suicide terrorism (e.g. suicide bombing) that is sanctioned by some cultural minorities and political groups in the modern world. Within our own culture built on the promise of attaining the American Dream, we struggle to fathom the appeal of suicide terrorism. Yet in Palestine, it’s said that some young people excluded from such opportunity instead aspire to become the kind of “martyrs” that are culturally celebrated in songs, posters, and trading cards. While those of us in the West view seppuku and martyrdom as incomprehensible acts of suicide or murder-suicide, they are regarded as something altogether different in the cultures that sanction them. If that seems morally bankrupt, consider how we think of murder here in the U.S. While most would be quick to categorize murder as morally unacceptable, many view abortion, capital punishment, and killing in the context of war as perfectly justified.
An examination of such cultural relativism helps us to see how different meanings can distinguish an act of honor, self-determination, or self-sacrifice from an act of morally unacceptable suicide. But how do we account for the apparent absolutism of moral judgments in which individuals can’t see beyond their own moral perspective? Harvard psychologist Joshua Greene gives us some hints in a 2003 paper called “From Neural ‘Is’ to Moral ‘Ought’: What Are the Moral Implications of Neuroscientific Moral Psychology?”2 when he suggests that most people are “moral realists” who typically view morality as a set of inherent and immutable truths (although I haven’t read it, I suspect he does the same in his more recent book Moral Tribes: Emotion, Reason, and the Gap Between Us and Them). In contrast, a neuroscience perspective argues against moral realism, recognizing instead that moral judgments are defined by social context and governed by specific regions of the brain. Research with people who have sustained brain injuries has revealed that those with damage to brain areas like the ventromedial prefrontal cortex often have significant difficulty with psychological tasks that measure moral decision making ability. In other words, morality is subject not only to cultural relativism but also brain relativism (for a good review of the evolving complex neuroscience of morality, see “The Neural Basis of Human Moral Cognition” by Jorge Moll and colleagues3). Inasmuch as moral reasoning is mediated by specific anatomical brain circuits, it isn’t surprising that moral judgments might differ between individuals.
While traditional approaches to moral philosophy have emphasized the role of rational thinking in moral decision-making, modern neuroscientific perspectives recognize that moral judgments also involve intuitive and emotional or “gut” reactions. This may help to explain why individuals tend to have a reflexive aversion to the word “suicide” and react to culturally foreign acts like suicide terrorism with moral indignation and disgust. In their paper, “Psychology Out of the Laboratory: The Challenge of Violent Extremism,”4 psychologists Jeremy Ginges, Scott Atran, and their colleagues describe how people who participate in suicide terrorism don’t act out of the kind of reasoning that analyzes risk and benefit, but rather “deontic reasoning” based on moral imperatives and “sacred values.” According to this view, devotion to principles like honor, revenge, sacrifice, or self-determination can sometimes trump any reasoned consideration of the negative consequences of suicide. In much the same way, emotional attachment to our own individual moral values seems to predict how we react to the question of whether suicide might sometimes be acceptable. Consistent with this idea, a psychological experiment published in a paper called “Tainting the Soul: Purity Concerns Predict Moral Judgments of Suicide” by Joshua Rottman and colleagues concluded that people’s views on the immorality of suicide seems to be determined by emotional concerns about the violation of our souls.5
Examining suicide through the lens of cultural and moral relativism reveals some important things that are often missed when taking about suicide. First, not everyone thinking about suicide is irrational or “crazy.” Second, strong differences in opinion over the morality of suicide are unavoidable. Finally, and perhaps most importantly, moral judgments about suicide can change. Accepting the moral relativism of suicide doesn’t mean that we should discard morals altogether however. As Joshua Greene writes, “giving up on moral realism does not mean giving up on moral values.”2 In fact, a neuroscientific view of morality suggests that our brains may be hard-wired for intuitive, emotional moral judgments because morality was a crucial evolutionary development for survival in social groups. In other words, neuroscience recognizes that we depend on moral judgments for our very existence. Therefore, the answer to the question, “when is suicide acceptable?” isn’t that it’s “OK” whenever people think it is. On the contrary, from a moral perspective, we should still try to prevent suicide whenever we can.
In a recent episode of the podcast Radiolab, Cuban-exile Vladimir Ceballos was asked about why a member of the 1980’s counter-culture movement Los Frikis deliberately injected himself with HIV-laden blood. Ceballos explained it this way: “Death is a door. When you don’t have any more doors to open, death is a door.” Preventing suicide is therefore about finding other doors when it seems like there are none. When patients with depression conclude that suicide is the only way out of an intolerable existence, it’s up to mental health professionals to help them find a light at the end of melancholia’s dark tunnel. Palliative care clinicians can offer other options like hospice care, pain management, and palliative sedation to those at the end of life contemplating euthanasia. In a similar fashion, pragmatic solutions to the problem of suicide terrorism depend on the development of viable alternatives.
Lately, the term “rational suicide” has gained traction as a way of removing automatic associations between suicide, psychiatric disorder, and irrational thinking in favor of a view that suicide in certain contexts might be understandable or even reasonable. But the concept of rational suicide is inherently flawed, because even when mental illness is present, there’s almost always an internal logic to suicide, if not widespread agreement that it’s the best or only option for a given situation. Finding alternatives to suicide first requires an understanding of the rationale and moral meaning of taking one’s life, which must then be transformed within an individual or within a sanctioning culture in order to find a new path.
References
1. Pierre JM. Culturally sanctioned suicide: Euthanasia, seppuku, and terrorist martyrdom. World Journal of Psychiatry 2015; 5:4-14.
2. Greene J. From neural ‘is’ to moral ‘ought’: what are the moral implications of neuroscientific moral psychology? Nature Reviews Neuroscience 2003; 4:846-850.
3. Moll J, Zahn R, de Oliviera-Souza R, et al. Nature Reviews Neuroscience 2005; 6:799-809.
4. Ginges J, Atran S, Sachdeva S, Medin D. Psychology out of the laboratory: the challenge of violent extremism. American Psychologist 2011; 66:507-519.
5. Rottman J, Keleman D, Young L. Tainting the soul: purity concerns predict moral judgments of suicide. Cognition 2014; 130:217-226.




