Addiction
Breaking the Chains of Addiction
Stop compulsive behavior by navigating your "tipping point."
Posted July 31, 2022 Reviewed by Abigail Fagan
Key points
- A protein called FosB produced in the brain may enhance compulsive behavior and motivation.
- Emotions can serve to fuel the intensity of compulsive behaviors.
- Enhancing your emotional precision by understanding the S-REF model can help diffuse "justifying" thinking.
- Engaging the "tipping point" of emotional intensity can breach the temptation to engage compulsive responses.
“It feels like I have zero control when the urge strikes.”
“I always come back to it and it's ruining everything.”
“I like the way it makes me feel at first, but then I am left sad and depressed.”
“I know it’s wrong and bad for me in so many ways, but I just can’t stop.”
This is how some of my patients have described their feelings about their addictions or compulsions. Compulsive behaviors can manifest in the form of mood-eating, porn use, internet (doom-scrolling), sex, social media, exercise, gambling, or psychoactive substance engagement such as stimulants, depressants, opiates, and hallucinogens (Gomez et al., 2022). Whatever form it takes, when a person develops a compulsion, the brain’s inhibitory response process (ability to stop) becomes greatly compromised, and thus, many succumb to their overwhelming emotional impulses.

In fact, research concerning the role of an implicated protein called FosB expands our understanding of how the brain is further stimulated and learns to adapt in response to repeated behaviors, thus instigating the likelihood of compulsive engagement repeating itself the next time. Think of a stack of bricks (FosB), one placed on top of the other, creating layers of this protein. This engagement behavior to stimuli you are drawn to builds upon and reinforces the stability and strength of FosB, making it even harder to break the chain of compulsion.
As well, FosB may promote motivation and reward processes in the brain, thus serving to incentivize repeat performances with a stronger tenacity (Nestler, 2015). But stopping the number of activations, or what is known as ‘hedonic processing,” is similar to removing each brick, one by one, until ultimately, FosB has been reduced greatly in accord with that specific compulsion (Harris et al., 2007).
How emotions serve to fuel compulsive behaviors
Emotional regulation is the “ability to exert control over one’s own emotional state.” For those who find themselves in addictive circumstances, this can be extremely difficult to control because our emotions can depict an array of things about how we are feeling such as lonely, afraid, sad, chaotic or overwhelmed and more. When we experience negative emotional states, executive function recedes. The “executive” part of the brain is responsible for executing skills like attention, reasoning, judgment, problem-solving, creativity, emotional regulation, and impulse control (Scott et al., 2022). Notice the words reasoning, regulation and impulse control, as they are the forerunners of processes required for abating compulsive responses. When this part of our brain is eclipsed by emotion, it is a challenge to think logically and rationally, thus, emotional reasoning takes over.
Enhancing emotional precision
One of the first questions I ask patients who reveal an issue with addiction or compulsion is if they can name the precursory feeling that occurred right before they decided to engage in the substance, thing or activity that is the issue. They may describe feeling alone, sad, angry, hopeless, unappreciated, or even bored (Koob, 2015). These “feeling states” predominate our limbic system and the structures buried deep within it can influence associative responses from memories where relief came through something one may have formerly indulged in the past (“The Limbic System,” 2019). This can enhance the motivation for organized responses that previously led to immediate gratification.
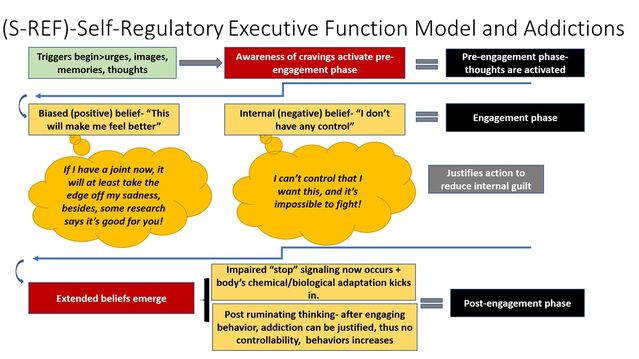
However, by asking patients to identify the primary and overriding feeling they were experiencing right before they sought out relief, we can learn to understand and distinguish the primary triggering emotion from the vast range of emotional colors at hand. And once we understand this emotional baseline, patients can learn strategies for controlling their irrational emotional narratives (scripts to justify addictions) to foster better outcomes (Komulainen et al., 2021). This can be seen below in what authors Spada et al, (2015b) have explained as an S-REF model of thinking, where beliefs lead to erroneous appraisals of situations and intrusions become less likely to be dealt with appropriately. Below is an example of how I see this model carried out in patients with addictions or compulsive behaviors.
Recognizing the “tipping point” and modifying the moment
Author Malcolm Gladwell presented the idea of the "tipping point" as the threshold or moment of greatest critical mass (Gladwell, 2005). To borrow on this idea, when it comes to addictions, the “tipping point” is that moment where emotions and thoughts begin to subsume the person, initiating swift propositions for the fastest way to reduce emotional intensity, usually in the form of negative and unhealthy behaviors. I teach patients to understand this mechanism because it offers the greatest potential for overriding the automaticity (auto-response reaction) of addictive or compulsive temptations (Vuilleumier, 2015). It is not an easy task by far, because the tipping point for engaging in addictive or compulsive habits is mere milliseconds, and the “pleasure” activation switch in the brain is flipped quickly.
Ways to break the tipping point moment
1. Counting
When feelings arise that are identified as triggers, try taking a moment to visualize something completely different that requires front-brain focus. I help train patients to enact active imagery which in turn jumpstarts neural activation (Sambuco et al., 2022).

Imagine a film reel counting down from 10 back to 1, holding the shifting image for 10 seconds, which may be long enough for you to gain some breathing room and disengage prior thoughts, thus reclaiming some homeostasis. This can be done as many times as needed.
2. Stay front-brain
Going for a walk, a run, building a puzzle, doing some house cleaning, mowing the lawn, calling a friend, or reading fiction — all can help move you back to the front-brain.
3. Spitting in the soup
Our brains may seek out what is “pleasurable” or “relieving” in a moment of weakness. But what if we made the activity less pleasurable? For a smoker, it might be that they supplement yogurt with pineapple, or milk, before they smoke. Yogurt and pineapple can create a negative taste alteration that may create an aversion to reaching for a cigarette. For those with compulsive porn use, breaking the “illusion” by reading some of the hard narratives of women and men who have had the courage to expose horrible elements of the porn industry can be a powerful demotivator. Creating aversions by pairing a counter-potential can help challenge an addiction.
Ultimately, breaking the chain of addiction and compulsion requires our full conviction, and we have to want to be free of it before we ever start trying.
References
Gladwell, M. (2005). The Tipping Point: How Little Things Can Make a Big Difference (Abridged ed.). Little, Brown & Company.
Gomez, R., Stavropoulos, V., Brown, T., & Griffiths, M. D. (2022). Factor structure of ten psychoactive substance addictions and behavioral addictions. Psychiatry Research, 313, 114605. https://doi.org/10.1016/j.psychres.2022.114605
Harris, G., Hummel, M., Wimmer, M., Mague, S., & Aston-Jones, G. (2007). Elevations of FosB in the nucleus accumbens during forced cocaine abstinence correlate with divergent changes in reward function. Neuroscience, 147(3), 583–591. https://doi.org/10.1016/j.neuroscience.2007.04.050
Komulainen, E., Glerean, E., Heikkilä, R., Nummenmaa, L., Raij, T. T., Isometsä, E., & Ekelund, J. (2021). Escitalopram enhances synchrony of brain responses during emotional narratives in patients with major depressive disorder. NeuroImage, 237, 118110. https://doi.org/10.1016/j.neuroimage.2021.118110
Koob, G. F. (2015). The dark side of emotion: The addiction perspective. European Journal of Pharmacology, 753, 73–87. https://doi.org/10.1016/j.ejphar.2014.11.044
Nestler, E. J. (2015). ∆FosB: A transcriptional regulator of stress and antidepressant responses. European Journal of Pharmacology, 753, 66–72. https://doi.org/10.1016/j.ejphar.2014.10.034
Sambuco, N., Bradley, M. M., & Lang, P. J. (2022). Narrative imagery: Emotional modulation in the default mode network. Neuropsychologia, 164, 108087. https://doi.org/10.1016/j.neuropsychologia.2021.108087
Scott, J.G., Schoenberg, M.R. (2011). Frontal Lobe/Executive Functioning. In: Schoenberg, M., Scott, J. (eds) The Little Black Book of Neuropsychology. Springer, Boston, MA. https://doi.org/10.1007/978-0-387-76978-3_10
Spada, M. M., Caselli, G., Nikčević, A. V., & Wells, A. (2015b). Metacognition in addictive behaviors. Addictive Behaviors, 44, 9–15. https://doi.org/10.1016/j.addbeh.2014.08.002
The limbic system. (2019, January 24). Queensland Brain Institute - University of Queensland. https://qbi.uq.edu.au/brain/brain-anatomy/limbic-system#:%7E:text=The%2….
Vuilleumier, P. (2015). Precision about the automatic emotional brain. Behavioral and Brain Sciences, 38. https://doi.org/10.1017/s0140525x14001046




