Genetics
Scientific Fraud About Brain Scan Findings
Psychiatrists wrongly assume that all brain scan differences are abnormalities.
Posted July 14, 2014
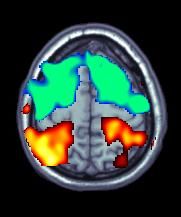
One way that some "biological" psychiatrists twist the truth in order to justify their belief that certain behavioral problems are due entirely to brain disorders involves the neuroscientists' new toy, the Functional MRI (fMRI) brain scan. fMRI machines, because they measure magnetic fields, can map both brain structure and brain function because the iron in blood that passes through the brain creates a magnetic field. If a section of the brain has increased activity, blood flow there increases, and it lights up on the scan.
In this post I will not be talking about gross findings that affect the entire brain, like the shrinkage (cerebral atrophy) seen in advanced Alzheimer's and in some cases of severe advanced schizophrenia (and yes, contrary to what the anti-psychiatry folks say, that was found in 30 studies of patients with schizophrenia who had never taken antipsychotic medications). Those findings are clearly indicative of disease. What I will be talking about in this post are changes in small brain structures that are often involved in specific mental tasks.
What researchers do is to use fMRI to compare certain brain structures and brain activity, particularly in the primitive part of the brain called the limbic system, in some diagnostic group with matched controls who do not have the disorder. For instance, an important brain structure called the left amygdala is smaller, on average, in subjects who exhibit the signs of borderline personality disorder (BPD) than in subjects who do not have the disorder.
Of course, they are comparing averages, so the left amydala in some BPD patients is larger than those of the average control. Notice also that the scientists only occasionally compare different diagnostic with each other. Differences in amygdalar size and activity are found in any number of different diagnostic groups in psychiatry.
Another way of saying this is that the observed differences may be non-specific and therefore only peripherally related to the diagnosis in question.
The more annoying source of misleading conclusions is that whenever a difference is found between a diagnostic group and controls with no mental disorder, that difference is automatically labeled an abnormality. If a patient has an abnormality, then of course they must have a brain disease. Or so goes the reasoning.
Actually, these scientists do not know if what they have found is an abnormality or not. What makes the use of the term abnormality totally misleading is that the brain, particularly in terms of limbic system structures, is plastic. This means that, in the normal brain, these structures can change in size to reflect activities that become important to a given individual. Such changes can be very quick and substantial.
For example, in the February 2010 issue of the Archives of General Psychiatry (Volume 67 [2] pp. 133-143), Pajonk, Wobrock, Gruber et. al. found that after just three months of a vigorous exercise program, the size of a brain structure called the hippocampus increased an average of 16 percent in "normals!"
It is also true that the part of the brain that controls finger movements is, on average, much larger in concert violinists than in non-musicians. The conclusions that the so-called biological psychiatrists would be, I guess, that both being a concert violinist and engaging in vigorous exercise are diseases!
Another point that should be obvious: Certain parts of the brain become more active when you engage in certain activities. For example, certain parts of the brain light up when you try to solve a Rubik's Cube that don't light up if you are, say, working a crossword puzzle. The biological psychiatrist's conclusion? Doing a Rubik's Cube must be a disease! Oh, wait a second–maybe it's doing the crossword puzzle that's the disease and doing the Cube that is the normal?
Certain areas of the brain are important in serving as a sort of early warning and response center for the brain to both danger signals and to important social signals. These areas are called the amygdala, the anterior cingulate gyrus, and the orbital frontal cortex. Neural pathways that encode early patterns of social attachment, social stimulus appraisal (social cognition), and fight or flight responses to fear are all centered in these areas.
Damage to the amygdala in monkeys leads to impairment in their ability to respond appropriately to the approach of other monkeys. Monkeys thusly impaired cannot tell whether other monkeys are coming to attack them or to mate with them.
Responding quickly to both environmental dangers and social cues has important survival value. If we had to stop and think each time we were confronted with commonly encountered situations, we would be nearly paralyzed. Therefore, much of our habitual behavior in social situations as well as our fight or flight response to fears is set in motion by the neural pathways in these brain areas. The thinking parts of the brain can override the initial response, but they do not kick in until after the habitual responses are first triggered.
Long term adaptive changes and conditioned responses that cause different parts of the brain to change usually begin to take place at the level of the synapse, the part of nerve cells which touches and communicates with another nerve cell. There are probably many mechanisms by which neuronal pathways become altered. Gene expression is literally altered because of input from the environment. This is called epigenetics.
Another important concept is long term potentiation, which I will discuss briefly.
An increase in the strength of a synapse occurs through this process. What this means in a nutshell is that stimulating a given synapse once or twice does not lead to changes in its strength. However, when a synapse is stimulated more than that, new proteins are produced in the neuron on the receiving end of the synapse that lead to a more permanent increase in the strength of the synaptic connection. This strengthening happens not only in the one synapse but in other nearby synapses.
If a synapse is not stimulated over a long enough period, it can weaken and then literally disappear. Use it or lose it.
Now back to epigenetics. This refers to the process by which outside environmental input turns genes off and on. The vast majority of genes in any cell are in the “off” position–including genes that affect the way neurons work. Most genes are accompanied by other genes whose entire function is to turn them off and on in response to environmental factors.
Examples of mechanisms that produce such changes are DNA methylation and histone modification, each of which alters how genes are expressed without altering the underlying DNA sequence. Childhood experiences such as trauma have been shown to lead to epigenetic changes in several brain areas, but these changes may be amenable to alteration by psychotherapy and therefore reversable.
The point of all this is that some “differences” between groups on fMRI scans may be due to disease, but they may also instead be due to certain brain functions being engaged by the subjects differently during the experiment. More importantly, the differences may also just be conditioned responses to a particular environment in which the subjects have spent a long time. fMRI findings alone do not tell us which of these three possibilities is being represented by any observed "differences."
In order to differentiate true brain pathology from conditioned responses, good scientists will look at a variety of other factors and then make their best guess based on a preponderance of the evidence. Schizophrenia, for example, is almost undoubtedly just as much a brain disease as Alzheimer’s disease. For one thing, in addition to the cerebral atrophy often seen in advanced cases, there are a huge number of highly diverse brain scan differences in smaller brain areas between people who have this disease and people who do not, although none by itself is necessary or sufficient to produce the condition.
Some of these differences, like differences in areas controlling eye movements, do not seem related to the symptoms of the disorder. This makes it less likely that the observed differences are just a matter of normal brain functioning as it works on a specific task.
What I consider the most important way to distinguish a finding due to a brain disease from other causes involves the concept of persistence and pervasiveness. Memory problems from Alzheimer’s disease and delusions from schizophrenia, for example, may get slightly better or worse at difference times, but they are always present to a significant degree no matter the environment for a significant length of time.

The symptoms of most people with ADHD, on the other hand, seem to completely disappear under certain environmental conditions. Kids with this diagnosis used to frequent noisy video arcades with multiple distractions and yet be able to concentrate just fine there. Real brain diseases do not just evaporate like that.
Doctors who like to insist that ADHD is a true disease would explain this away using the most incredible pseudo-logic imaginable, with “facts” that have absolutely no scientific basis and were basically pulled out of their you-know whats. Somehow video arcade concentration, they would say, is not concentration! I've heard this said multiple times. Then what, pray tell, is it?




