ADHD
Race and ADHD
Race is highly relevant to research and clinical care for ADHD.
Posted June 10, 2020 Reviewed by Gary Drevitch
Discussions of ADHD, like discussions of mental and behavioral conditions generally, often are “race blind," yet race, along with culture, ethnicity, and social identity, is an important consideration in understanding ADHD.
Terms. No term is perfect, as different people like to refer to themselves in different ways. One common term for under-represented groups is person of color (or POC); another is BIPOC (Black, Indigenous, or Person of Color). With almost no research on African or Caribbean immigrants to the U.S., I use the term Black as a shorthand but it usually refers to research on African Americans; I use the term BIPOC to refer to other non-white groups for brevity. I emphasize research on Black Americans due to the current context and because it is the clearest. However, many conclusions apply to other BIPOC groups in the U.S.
Genetics and race. One of the enduring falsehoods about race is that it has biological meaning. We have seen this ugly untruth surface lately with suggestions that excess COVID-19 deaths among Black American and British communities relate to weak genetic immunity. That is scientific and biological nonsense. There is individual variation in genetic immunity. And some family lines for inherited conditions are more common in certain socially defined groups. But while individual risk is influenced by genetic liability, group differences in infectious disease outcome across socially-defined race groups is related to social factors—differential exposure, differential health care, and so on. This has been demonstrated many times. (Genetics can also trace ethnic lineages, but these bear little or no relation to what we call race.)
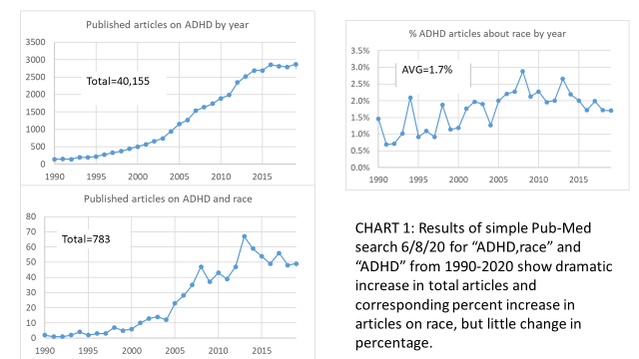
Bias in research and clinical care not yet overcome. Most research on ADHD is on boys of European-Caucasian ancestry in North America, Europe, and Oceana. When black children are included for representativeness, there usually is insufficient information to clarify if conclusions apply equally within the Black population. Relatively few studies specifically examine aspects of race or cultural variation, although there has been some increase as studies of ADHD have grown (see Figure).
In clinical care, biased decision-making is slowly being addressed—for example, by specific training to overcome implicit bias—but still persists. Thus, the entire health and mental sectors, not just ADHD, struggle to address racism, stereotyping, implicit bias, research representation, and care disparities. Black families are often reluctant to participate in research due to mistrust. Tuskegee may seem ancient history to Whites, but it very real for the Black community. Mistrust of research is also fueled by ongoing experiences of discrimination in research and health care settings.
Overall, despite some progress, we remain woefully short of knowledge about the specific needs of Black and other highly diverse BIPOC communities. With that caveat in mind, here are a few things recent studies have reported specifically about ADHD.
Racism and stereotyping affect behavior. American youth are increasingly concerned about societal racism. Their feeling of exposure to incidents of public racism and discrimination are rising. Obviously this has been amplified in recent weeks. Over time, the sometimes daily exposure to discrimination and prejudice experienced by Black and other BIPOC groups are associated with subsequent increase in symptoms of depression and ADHD, as well as higher likelihood of trying alcohol, tobacco, or marijuana. It is also associated with higher blood pressure by adulthood. Even in preschool, children are acutely aware of stereotypes about gender and race. Young people and adults alike are sensitive to social stereotypes. For example, if someone thinks they are activating a stereotype (a woman struggling on a math test, a Black youth struggling on a national educational progress test) then their blood pressure goes up and their performance noticeably deteriorates. Such stereotype threat is well-established as an issue in educational settings. Yet its effects on referral and diagnosis are largely unstudied for ADHD and learning disorders in Black youth.
Trauma and social disadvantage are related to ADHD. Children who are BIPOC in the U.S. are generally exposed to more social adversity than children in the majority culture. ADHD worsens in these contexts. Thus, separating social adversity effects from ADHD itself is a greater challenge in these populations.
Rater “bias,” while not as invalidating as some worry, still is notable in ratings of the same videotaped behavior across races. Factors affecting ratings include role, setting, past experience of discrimination, acculturation, identity, race of rater, race of child, and sex of child. (Ratings are not much affected by prior experience of ADHD or valuing certain expressive styles). In the real world, African American parents rate their children as higher on ADHD symptoms than White parents do. It is unclear why—different parent tolerance, different child behaviors, or other factors. Fortunately, some standardized assessment measurements take this into account, with national norms for Black children.
Appropriate parental and teacher strategies for ADHD and disruptive child behaviors are well known for Caucasian children in majority settings. The extent to which these apply for Black and other cultural groups remains an active and controversial area of study. In some studies, the most appropriate parenting style for positive outcome for children differs by race.
Some basic facts:
- In random household surveys using formal diagnostic procedures, ADHD has the same prevalence in White and BIPOC groups.
- But in actual clinical practice, ADHD is under-identified in Black versus White groups. (It is unclear if it is under-identified in Black groups, or over-identified in White groups).
- When they do get treatment, Black youth are more likely than White to discontinue treatment or use it only intermittently, doubtless for multiple reasons not well studied.
Recommendations:
If you are in an under-represented minority group trying to understand if your child has ADHD, recognize that yes, he or she might. True incidence is about the same across racial groups in the United States. But the diagnostic process is complicated by race and stereotype effects as well as by a history of discrimination in many prior experiences of Black or BIPOC individuals to which a clinician has to be sensitive for an effective evaluation.
Your clinician should be mindful of race-specific norms, should consider the potential for implicit bias (unconscious stereotype uses even by the well-meaning; a tendency to over-diagnose conduct disorder in African American youth, and so on) which can affect everyone’s perception of the child, and should consider social dynamics: Is this child isolated, traumatized, or exposed to other important contexts? Finally, careful attention should be paid to impairment—that is, are the ADHD symptoms really interfering with the child’s development? A further caution: The diagnosis of conduct disorder should be scrutinized very carefully before it is applied to African American children, as it is over-applied.
Clinical practices for ADHD for children in BIPOC groups:
- Obtaining standardized ratings using multiple informants (best practice anyway).
- When possible, use norms for the child’s social group (increasingly available).
- Get objective evidence of impairment (grades, classwork, and class observation).
- Be cautious of possible over-diagnosis of conduct disorder in younger boys.
On the science side, we can’t yet be sure that ADHD criteria identify the same children across race and ethnicity. Some evidence says yes, some says not quite. So, racism and stereotyping can’t be ignored if we, as a still white-normed society, are to accurately help all children with ADHD and ADHD-like symptoms with valid evaluation of ability and needs and appropriate supports. For ADHD, it is very important to continue to learn about rater effects across race groups and to evaluate the validity of different ADHD correlates across populations.
Please note: Dr. Nigg cannot advise on individual cases for ethical, legal, and logistical reasons.
References
Coker TR, Elliott MN, Toomey SL, Schwebel DC, Cuccaro P, Tortolero Emery S, Davies SL, Visser SN, Schuster MA. (2016). Racial and Ethnic Disparities in ADHD Diagnosis and Treatment. Pediatrics. 2016 Sep;138(3).
DuPaul GJ, Fu Q, Anastopoulos AD, Reid R, Power TJ. ADHD Parent and Teacher Symptom Ratings: Differential Item Functioning across Gender, Age, Race, and Ethnicity. J Abnorm Child Psychol. 2020;48(5):679‐691. doi:10.1007/s10802-020-00618-7
DuPaul GJ. Adult Ratings of Child ADHD Symptoms: Importance of Race, Role, and Context. J Abnorm Child Psychol. 2020;48(5):673‐677. doi:10.1007/s10802-019-00615-5
Hales CM, Kit BK, Gu Q, Ogden CL. (2018). Trends in Prescription Medication Use Among Children and Adolescents-United States, 1999-2014. JAMA. 2018 May 15;319(19):2009-2020
Ji X, Druss BG, Lally C, Cummings JR. (2018) Racial-Ethnic Differences in Patterns of Discontinuous Medication Treatment Among Medicaid-Insured Youths With ADHD. Psychiatr Serv. 2018 Mar 1;69(3):322-331.
Kang S, Harvey EA. Racial Differences between Black Parents' and White Teachers' Perceptions of Attention-Deficit/Hyperactivity Disorder Behavior. J Abnorm Child Psychol. 2020;48(5):661‐672. doi:10.1007/s10802-019-00600-y
Leventhal AM, Cho J, Andrabi N, Barrington-Trimis J. (2018). Association of Reported Concern About Increasing Societal Discrimination With Adverse Behavioral Health Outcomes in Late Adolescence. JAMA Pediatr. 2018 Aug 20
Miller TW, Nigg JT, Miller RL. (2009). Attention deficit hyperactivity disorder in African American children: what can be concluded from the past ten years? Clin Psychol Rev. 2009 Feb;29(1):77-86.
Scharff, D. P., Mathews, K. J., Jackson, P., Hoffsuemmer, J., Martin, E., & Edwards, D. (2010). More than Tuskegee: understanding mistrust about research participation. Journal of health care for the poor and underserved, 21(3), 879–897. https://doi.org/10.1353/hpu.0.0323
Slobodin O, Masalha R. Challenges in ADHD care for ethnic minority children: A review of the current literature. Transcult Psychiatry. 2020;57(3):468‐483. doi:10.1177/1363461520902885
Spencer SJ, Logel C, Davies PG (2016). Stereotype threat. Annual Review of Psychology, 67, 415-437.
Yetter G, Foutch VM. (2017). Comparison of American Indian and Non-Native BASC-2 Self-Report-Adolescent Scores. Am Indian Alsk Native Ment Health Res. 2017;24(3):14-38.




