Anxiety
Groovy Probiotics
Are the beasties in your belly communicating with your brain?
Posted June 9, 2012
We've been told yogurt is good for us. And in times past, most cultures have traditions of fermented food, such as sauerkraut, kimchi, kefir, and a tasty tea-based drink I've been fermenting at home, called kombucha. All these foods are jam-packed with living yeast and bacteria species that go down your gullet to comingle with the one hundred trillion (yes, trillion) bacteria already living there.
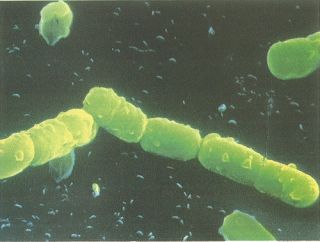
90% of the cells in your body are the bacteria who live on and within you. Most of them live in your colon. The species of bacteria in your colon could determine how thin or fat you are, or maybe how vulnerable you are to stress. The commensal beasties are difficult to study as they don't live outside the human gut and can't be cultured in a lab. There's a lot to learn.
So fermented food had an obvious advantage in that it kept longer in the days before refrigerators, but did it have another advantage perpetuating it's existence in so many cultures in human history? Are the probiotics helpful in keeping the beasties in our gut happy and healthy? I've discussed this issue a bit in a previous post, but last year a new paper came out that is also interesting:
Probiotics function mechanistically as delivery vehicles for neuroactive compounds: Microbial endocrinology in the design and use of probiotics.
The down-low is that probiotics are thought to modulate the production of inflammatory particles (cytokines), affect how well pathogens stick to the walls of our gut, and other groovy things. However, no one really knows how they do what it is that they do. There are now several studies with intriguing evidence that probiotics can affect the brain. One study even showed anxiety reduction in human volunteers (and mice) with administration of Lactobacillus helveticus and B. longum. Again, since disorders that affect the gastrointestinal tract seem to co-exist quite frequently with anxiety, depression, and other mood disorders, probiotics and gut health may have "profound clinical implications."

As I mentioned earlier, there is a great deal we don't know. As the organisms can't be cultured, it's difficult to study the secret life of the wee beasties while the host is walking around doing the day to day. There are zillions of varieties of beasties, and typically the probiotics used for studies depend on what company is supplying them rather than a more specific rationale or knowledge of the effects of each species,
So what, exactly, do we know? As far back as 1929 it was discovered that human carriers of certain Clostridium species who were given epinephrine to treat hives died suddenly of gas gangrene (oops). For 60 years, it was thought the epinephrine somehow suppressed the immune system, leading to the sudden fulminant infection. In the early 1990s, however, it was found that yes, indeed, gut bacteria could respond directly to human neurochemicals (such as epinephrine). It has been further proven (with the flurry of recent papers) that the communication between the beasties and the brain is a two way street. Neurochemicals are highly conserved in evolution - bacteria, plants, insects, and fish all produce forms of the neurochemicals called the catecholemines. Thus it makes sense that bacteria in our gut can communicate directly with using, to some extent, the same "language" as our mammalian brains.
Lactobacillus and Bifidobacterium species are known to produce GABA. Escherichia, Bacillus, and Saccharomyces produce norepinephrine. Candida, Streptococcus, Escherichia, and Enterococcus produce serotonin. Bacillus and Serratia produce dopamine, and Lactobacillus species produce acetylcholine. That's pretty much the entire hit parade of major neurotransmitters (there's histamine and glutamate and a few others - and histamine is known to be produced by some bacteria that infect shellfish, for example, causing food poisoning).
The most interesting case here is GABA, the major inhibitory neurotransmitter in the nervous system (it chills things out)--and there are whopping amounts made by the bacteria in fermented foods, and is also found in yogurt and typical probiotic capsules. GABA also turns out to be anti-inflammatory in the gut itself, decreasing the release of inflammatory cytokines. Thus there is a plausible mechanism by which certain probiotics could decrease inflammation and aid symptoms of conditions such as irritable bowel syndrome, and, considering the vagus nerve and all it's tendrils in the gut, have direct communication via the neurotransmitter GABA to the brain.
The author of the paper outlines some straightforward methods by which the individual effects of the probiotic species could be systematically characterized and studied. He has developed a framework for the promising new field of microbial neuroendocrinology. Of course his interest is along the lines of mining microbes for human use--it seems to me our ancestors and their fermented traditions have been mining microbes for these uses for some time, without all the species typing and science.

You have to be careful when you ferment and can foods at home, as pathogenic bacteria can live in your food along with the healthy probiotics. However, you can buy probiotics, or commercial yogurts with live active cultures, and kefir is available at most regular grocery stores. I like making kombucha, and I think as long as you use clean jars, clean hands, and freshly boiled or commercial ingredients, it is pretty safe. But who knows what the kombucha I drink is saying to my brain? There has to be more research to figure that out.
Copyright Emily Deans, MD




