Omega-3
SARS-COV-19: Fiber And Fish Oil Provide Prevention
Part 6: Fermentable fiber and DHA strengthen mitochondria and antiviral immunity
Posted July 9, 2020
Dietary fiber and its fermentation products, especially, the short chain fatty acids (SCFAs) acetate, butyrate, and propionate, have numerous beneficial effects. They can ameliorate chronic inflammatory diseases, improve immune responses beyond the gastrointestinal system, such as influencing the lung and brain, dampen immune responses, act on immune cells such as regulatory T cells, dendritic cells, neutrophils, macrophages, memory responses of CD8+ T cells, and T helper cell differentiation. SCFAs can influence metabolism in liver, muscle, immune cells, and adipose tissue (1). Fermentable fiber studies (i.e. inulin) with humans and mice found that the high fiber diet (HFD) specifically increased colon or gut bacteria with SCFAs that reduced type 2 diabetes symptoms as measured by glucose tolerance tests and hemoglobin AIC. When the stools from both patient groups was transplanted into germ-free mice, those receiving stool from the HFD patients had the best outcomes. These findings reinforce the importance of the gut microbiota, or all the organisms inhabiting the human digestive tract, as the mediator of health and change (2).
The enzymes in the mouth and upper small intestine such as amylase and ptyalin cannot digest prebiotic fibers such as inulin which pass relatively unchanged to the large intestine where they are fermented into SCFAs. Inulin is water soluble and found in many plants which use it to store energy in their roots instead of starch. Inulin has up to 10% the sweetness of sugar but only 25-35% of the food energy of sugar and starch with many added health benefits noted earlier. High performance inulin at 10 grams daily in type 2 diabetic women increased antioxidant capacity, while decreasing body weight and glycemic indices (3). A teaspoon is 4.2 grams and one twice daily would be essentially 10 grams. There are presently no studies with COV or COV-19 and a diet rich in fermentable fiber. People of Northern European ancestry are known to be more sensitive to inulin and could substitute the fermentable prebiotic for fermentable fiber Psyllium husk. Nevertheless, previous work with influenza regarding antiviral immunity and inulin consumption is instructive (1).
coordsize="21600,21600" o:spt="75" o:preferrelative="t" path="m@4@5l@4@11@9@11@9@5xe"
filled="f" stroked="f">
style='position:absolute;margin-left:-1.25pt;margin-top:473.9pt;width:411.95pt;
height:213.15pt;z-index:251659264;visibility:visible;mso-wrap-style:square;
mso-width-percent:0;mso-height-percent:0;mso-wrap-distance-left:9pt;
mso-wrap-distance-top:0;mso-wrap-distance-right:9pt;
mso-wrap-distance-bottom:0;mso-position-horizontal:absolute;
mso-position-horizontal-relative:margin;mso-position-vertical:absolute;
mso-position-vertical-relative:margin;mso-width-percent:0;
mso-height-percent:0;mso-width-relative:page;mso-height-relative:page'>
o:title=""/>
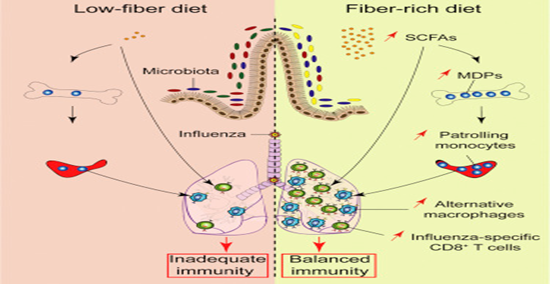
In mice born and raised on a low fiber diet, a control group supplemented with cellulose (a poorly fermentable diet) was compared to the test group on a high fiber diet (HFD) supplemented with inulin. Both groups of now adult mice were exposed intranasally to influenza A virus (IAV) which uses the same ACE-2 receptor as coronaviruses. HFD mice had prolonged survival and improved clinical scores. They also experienced reduced pulmonary resistance, related to milder airway constriction, increased elasticity and therefore better lung function. The control mice lungs’ had large accumulations of red blood cells in their lung tissue indicating destruction and vascular leakage. Other measures of immunopathology were decreased in HFD fed mice. Additional antiviral immunity effects of HFD with inulin (figure 1) included 1) alteration of the intestinal microbiota with increasing SCFAs especially butyrate. Moreover, “supplementing the drinking water with butyrate for 2 weeks prior to and throughout the infection resulted in protections similar to that elicited by a HFD”. 2) Prevention of excessive neutrophil (white blood cells) influx into the airways by decreasing CXCL1 (a potent neutrophil chemo attractant) produced by lung macrophages and monocytes. 3) Though there were more Ly6c- patrolling monocytes in the blood, bone marrow, and lungs, they were preferentially differentiated into alveolar and interstitial (between cells) macrophages with a less inflammatory “M2” phenotype also called “alternatively activated macrophages” (AAMs). This reduced airway neutrophils and damage (4). CD8+ T lymph cell activation occurred with specific anti-influenza viral effect and a high cytotoxic cell killing capacity was found (1). There are two types of CD8+ T cells. Memory T cells that have been previously exposed to an infectious agent or a foreign body that they know how to fight and “naïve” T cells which have never fought anything. Because we have had no exposure to COV-2 before, the memory T cells are not able to mobilize. The battle is left to the new “naïve” T cell troops. Fortunately, inulin activates these T cells with specific antiviral and high cytotoxic capacity making them potent viral killing T cells.
As Trompette and associates summarized (1):
… our data demonstrate that dietary fiber and SCFAs can protect against severe influenza infection by reducing tissue damage and by boosting adaptive anti-viral immunity. SCFAs have predominantly been associated with immunoregulation and the prevention of exaggerated inflammation; however, our work highlights a dual role of SCFAs. By tuning down excessive innate responses, promoting tissue-protective mechanisms, and stimulating specific adaptive immunity, dietary fiber and SCFAs can create an immune balance that ultimately protects against disease.
The importance of the microbiota in another study (4) is again revealed in their modulation and fine tuning of interferon which protects lung tissue in mice (all mammals) from viral infections. If the mice were given antibiotics which killed or disrupted the microbiota, their lung tissue was more easily infected by influenza. If the antibiotic-exposed mice were given fecal material of control mice orally by a tube to their stomach (fecal transplant), they became more resistant. That is, it increased production of interferon proteins with various antiviral function and fine-tuned interferon viral resistance. (Figure 2).
o:spid="_x0000_s1026" type="#_x0000_t75" style='position:absolute;
margin-left:94.4pt;margin-top:20.7pt;width:320.25pt;height:150.05pt;z-index:251660288;
visibility:visible;mso-wrap-style:square;mso-width-percent:0;
mso-height-percent:0;mso-wrap-distance-left:9pt;mso-wrap-distance-top:0;
mso-wrap-distance-right:9pt;mso-wrap-distance-bottom:0;
mso-position-horizontal:absolute;mso-position-horizontal-relative:margin;
mso-position-vertical:absolute;mso-position-vertical-relative:text;
mso-width-percent:0;mso-height-percent:0;mso-width-relative:page;
mso-height-relative:page'>
o:title=""/>

Omega 3 fatty acids are part of the cellular membrane of all human tissues including muscle and mitochondria. Fish oil omega 3s (FOO3s) from supplementation are incorporated into our cellular membranes (5). They can lower the mortality rate for people with cardiovascular disease (CVD). FOO3s can also regulate blood vessel lining cells (endothelial) by decreasing oxidative stress, atherosclerotic plaque formation, and inflammation. Even in mice fed a high fat lard diet, FOO3s supplementation resulted in a 54% decrease in plaque formation. It also increased nitrous oxide (NOS) release and endothelial NO synthase activity necessary for vascular health and sexual function. Additionally, it lowered the levels of mitochondrial oxidative stress and cytochrome C release reflecting improved mitochondrial health (6). FOO3s can interact favorably with fermentable fiber which produces butyrate (e.g. pectin, in apples) to increase mitochondrial energy production and the death of mouse colon cancer cells (5). When mitochondria are compromised by viral infection, they are no longer key (8) to regulating the apoptotic (cellular death) pathway whereby damaged cells are selectively eliminated (autophagy) that can contribute to cancer formation. FOO3s are a mixture of two polyunsaturated fatty acids, EPA and DHA, which together have been shown to decrease inflammatory states and modulate immune mechanisms including B cell activity. B cells are involved in antibody production and cytokine (regulate immunity and inflammation) secretion (9) which is enhanced in lean and obese mice by FOO3s (10).
There is evidence in rodent studies that DHA is more effective than EPA (10). Newly diagnosed diabetics have a decreased production of B cell cytokines and obese humans and mice (two of the risk factors for COVID-19) have a lower antibody response to influenza infection (utilizes same ACE-2 receptor) or vaccination. In these same mice, DHA improved “influenza-specific antibody production” (10). In a pilot human study, the high DHA fish oil supplement (0.5g EPA and 2.0 g DHA daily) increased isolated B cell cytokine secretion relative to base line, while olive oil and regular fish oil concentrate did not.
Specialized pro-resolving (lipid) mediators (SPMs) (11) which include resolvins, protectins and maresins (12) ameliorate inflammation by several mechanisms. This includes resolutions of inflammation from increasing anti and decreasing pro-inflammatory activity, respectively, supporting immune macrophages to remove dead and dying cells, or autophagy, and tissue regeneration. The SPMs are mainly derived from EPA (18-HEPE) and DHA (H-HDHA, 17-HDHA), but DHA provides small amounts of the precursors for the three SPMs noted, while EPA only contributes to the resolvins. An added benefit of DHA may be its benefit in brain health where it is concentrated more than 250 times higher than EPA (14). Moreover, brain neurogenesis is observed in rats even in older animals given DHA (15), which may be consistent with improved memory found in older individuals receiving DHA (16). However, more research is needed to clarify FOO3s beneficial interaction with fermentable fiber. How we can help our mental health and public policy is next in part 7.
This is not meant to be medical advice. The reader needs to consult their health care provider before making any medical decisions.
References
1. Trompette, A., Gollwitzer, ES., Pattaroni, C., et al: Dietary Fiber Confers Protection against Flu by Shaping Ly6c- Patrolling Monocyte Hematopoiesis and CD8+ T Cell Metabolism. Immunity. 2018 May 15;48(5):992-1005.e8. doi: 10.1016/j.immuni.2018.04.022.
2. Zhao, L., Zhang, F., Ding, X., et al: Gut Bacteria Selectively Promoted by Dietary Fibers Alleviate Type 2 Diabetes. Science 2018,359, 1151-1156.
3. Ryback, R.: Why French women don’t get fat? Unpublished manuscript.
4. Bradley, K. C., Finsterbusch, K., Schnepf, D., et al: Microbiota-Driven Tonic Interferon Signals in Lung Stromal Cells Protect from Influenza Virus Infection. Cell Reports. 2 July 2019, 28(1), 245-256. doi.org/10.1016/j.celrep.2019.05.105
5. Gerling, C. J., Mukai, K., Chabowski, A., et al.: Incorporation of Omega-3 Fatty Acids Into Human Skeletal Muscle Sarcolemmal and Mitochondrial Membranes Following 12 Weeks of Fish Oil Supplementation. Front Physiol. 2019; 10: 348. 2019 Mar 29. doi: 10.3389/fphys.2019.00348
6. Sun, R., Wang, X., Xia, M. Dietary Supplementation With Fish Oil Alters the Expression Levels of Proteins Governing Mitochondrial Dynamics and Prevents High-Fat Diet-Induced Endothelial Dysfunction. Br J Nutr. 2014 Jul 28;112(2):145-53. doi: 10.1017/S0007114514000701.
7. Fan, Y. Y., Vaz, F. M., Chapkin, R. S. Dietary Fat and Fiber Interactively Modulate Apoptosis and Mitochondrial Bioenergetic Profiles in Mouse Colon in a Site-Specific Manner. Eur J Cancer Prev. 2017 Jul;26(4):301-308. doi: 10.1097/CEJ.0000000000000263.
8. Baixauli, F., Acín-Pérez, R., Villarroya-Beltrí, C., et al.: Mitochondrial Respiration Controls Lysosomal Function During Inflammatory T Cell Responses. Cell Metab. 2015 Sep 1;22(3):485-98. doi: 10.1016/j.cmet.2015.07.020.
9. Waffarn, E. E., Baumgarth, N. Protective B cell responses to flu – no fluke! J Immunol. 2011 Apr 1; 186(7):3823–3829. doi: 10.4049/jimmunol.1002090
10. Guesdon, W., Kosaraju, R., Brophy, P., et al.: Effects of fish oils on ex vivo B-cell responses of obese subjects upon BCR/TLR stimulation: a pilot study. J. Nurt. Biochem. 2017, Nov 2, 53, 72-80. doi.org/10.1016/j.jnutbio.2017.10.009
11. Fattori, V., Zaninelli, T. H., Rasquel-Oliveira, F. S., et al.: Specialized pro-resolving lipid mediators: A new class of non-immunosuppressive and non-opioid analgesic drugs. Pharmacol Res. 2020 Jan;151:104549. doi: 10.1016/j.phrs.2019.104549.
12. López-Vicario, Cristina, Rius, B., Alcaraz-Quiles, J., et al.: Pro-resolving mediators produced from EPA and DHA: Overview of the pathways involved and their mechanisms in metabolic syndrome and related liver diseases. Eur J Pharmacol. 2016 Aug 15;785:133-143. doi: 10.1016/j.ejphar.2015.03.092.
13. Serhan, C. N.: Discovery of specialized pro-resolving mediators marks the dawn of resolution physiology and pharmacology Mol Aspects Med. 2017 Dec;58:1-11. doi: 10.1016/j.mam.2017.03.001.
14. Dyall, S. C.: Long-chain omega-3 fatty acids and the brain: a review of the independent and shared effects of EPA, DPA and DHA. Front Aging Neurosci. 2015 Apr 21;7:52. doi: 10.3389/fnagi.2015.00052.
15. Robson, L. G., Dyall, S., Sidloff, D., et al.: Omega-3 polyunsaturated fatty acids increase the neurite outgrowth of rat sensory neurones throughout development and in aged animals. Neurobiol Aging. 2010 Apr;31(4):678-87. doi: 10.1016/j.neurobiolaging.2008.05.027.
16. Lee, L. K., Shahar, S., Chin, AV, et al.: Docosahexaenoic acid-concentrated fish oil supplementation in subjects with mild cognitive impairment (MCI): a 12-month randomised, double-blind, placebo-controlled trial. Psychopharmacology (Berl). 2013 Feb;225(3):605-12. doi: 10.1007/s00213-012-2848-0.




