Health
The Frustrating Financial Realities of Therapy
Why finding and delivering mental health counseling is difficult.
Posted April 25, 2021 Reviewed by Lybi Ma
Key points
- High-deductible health plans can amount to sticker shock for patients, complicating the therapy process.
- Return requested paperwork promptly, readably, and completely to move off a waitlist to a scheduled appointment.
- Some insurers pay the same rates to therapists as 5-10 years ago. Others give paltry increases. Providers often drop these plans.
By December 2020, Gallup reported that Americans assessed their mental health at the lowest point in two decades.1
The New York Times featured “Nobody Has Openings”2 while Forbes aptly titled “We Need To Talk About Another Pandemic Mental Health Crisis: Therapist Burnout.”3
Both realities are troubling. One positive: telehealth acceptance was achieved in 60 days rather than the 10 years it may have taken without a pandemic to force it forward. Still, insurance companies pose challenges to members and providers.
High Deductible Health Plans (HDHPs) Amount to Sticker Shock
HDHPs, created to provide lower premiums but high deductibles, can provide a tax advantage if tied to a health savings account (HSA).4 They may also turn people away from help and pose problems.
Let’s assume a client, with few doctor visits, lab/medical tests, or prescriptions has a $4,000 deductible. Life turns stressful and the client schedules a therapy session, only to find out that he owes the provider $128 for the intake and $80-$125 ongoing, depending upon the session.5
If the client thought he’d pay zero or a co-pay, he’s gobsmacked. Guess who gets to deliver this news? Usually, the therapist, especially in small practices.
Best case: The client has anticipated the higher out-of-pocket expense and pays at the time of service. Worst case: He gets upset, the therapist chases payment, or never receives remuneration outside of collections. It's incredibly frustrating for all.
Understand your plan. Call the insurance company to ask what your “member responsibility” will be. Share this with your provider ahead of intake. Many clinicians ask about deductibles on provider paperwork.
Use an Employee Assistance Program (EAP). Some cases are more complex than a 45-minute EAP session allows, but most might be handled without cost to the client.

When you contact a provider, please disclose your intent to use EAP benefits with the exact EAP entity. Send a copy of the authorization on EAP letterhead or insist the EAP sends it directly to the therapist.
Return Requested Paperwork Promptly and Completely
Each week, therapists easily receive a dozen new appointment requests. If this was real estate, we’d call it a seller’s market because there aren’t enough openings to meet demand. Thus, therapists dutifully screen those best suited to their practices.
Return the required paperwork within two days of receiving it. You stand a better chance of getting on the schedule. If you send it back weeks later, that therapist has likely reached caseload capacity.
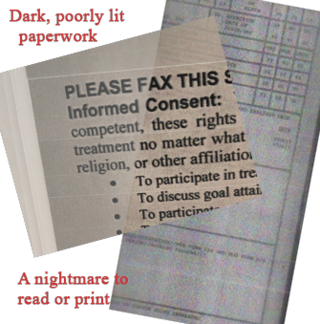
Those who return paperwork in shoddy condition may find themselves screened out in favor of those who made life easier on the administrative front.
Slanted camera pics with body shadows as you photograph it, with sloppy margins, print appallingly. Horribly. It's best to scan paperwork into a PDF using a scanner to enhance readability. Fax it, at an office supply store perhaps, to a provider’s HIPAA-compliant fax.
Barring a scanner, send a well-lit, no-shadows, nothing-in-the-margins image that preferably you have converted from a JPG to a PDF. Provide the front/back of your insurance card. You may not care about the backside info until your claim is denied and you must pay a session, in full. No worn-off letters or numbers, please. You can also use an app like Microsoft Office Lens, which straightens, trims, and converts JPG images into PDF form.
Answer questions posed—in paperwork or on a website—to provide a snapshot of your presenting concern, insurance/EAP you must use, and when you’re available. Be flexible there to land on the schedule vs. the waitlist.
Understand and Accept Practice Policies
All healthcare providers offer you “informed consent,” disclosing upfront policies (late cancellation/missed appointments), how to contact, and fees. Nothing sours a therapeutic relationship like money misunderstandings.
Miss a session or cancel late, and you will likely pay the full fee. Your insurance or EAP doesn’t pay for missed sessions. You do.
It’s a business reality due to the time set aside. The majority of clinicians work for-profit. Insurance pays only for session time.
If you or your child requires a higher level of care, your therapist may need to consult with other clinicians. This is not only helpful to treatment but mandated by ethics, state law, and insurance contracts.
Wise therapists set boundaries and charge for third party (school counselor/attorney) interaction, treatment coordination with facilities or providers, paperwork, even email, outside of quick scheduling or follow-up.
Drowning in Unrealistic Expectations and Paperwork
As the pandemic worsened, workers applied for unpaid, job-protected leave, under the Family and Medical Leave Act (FMLA) or disability and were sent to counseling. Disclose this upfront as you seek services. Expect to pay a fee.
Lawyers and professionals, including therapists, charge for time spent on a client’s case. This is a realistic expectation. Some unrealistic ones:
“Can’t we just email back and forth or chat on the phone?”
Therapy is a process that works in person or via telehealth audio and video. Your therapist must work by established rules and you must as well.
“Why do you charge other fees? I thought this was free.”
In addition to a desire to help, counselors earn a living and must face expenses to do so. Here’s the bottom line on a high-stress job, especially in a pandemic.
Per O*Net, the median annual income for mental health counselors was $47,660 or $50,000 for a metro area like the Washington metropolitan area. With more years in the field, counselors might earn $79-$89K, depending upon the region.6
It’s hard to tell if the numbers reflect expenses, let’s subtract $20,000 for average rent, utilities, slip/fall, and professional insurance; another $1,000 for professional dues, publications, and state fees; $1,000 for continuing education necessary to maintain licensure; and other expenses for computer, software, file storage, supplies for a total of $25,000, off gross income. At minimum.
No One Enters Mental Health Seeking Riches
Most clinicians expect, however, to get ahead yearly, just like you do.
Shocker: Two major insurers—top and bottom of the alphabet—have not improved rate structures in 5 to 10 years. That’s a fact. Forget the cost of living adjustment, experience, additional training. Insurers insist that therapists maintain physical addresses, increasing costs. Will telehealth change this? Many in the field have begun such advocacy.
Some insurance companies cater to stockholders, it may appear, rather than the effective delivery of mental health care. Their provider list may have newer, less experienced clinicians.
All scenarios explored here explains why therapists opt out of insurance altogether, and why there’s mounting frustration from those seeking treatment and those trying desperately to deliver it well.
Copyright @ 2021 by Loriann Oberlin. All Rights Reserved.
References
Find a therapist here.
5) Fees vary according to geographic region and insurance carriers. Some insurance carriers, including major, nationwide companies, have not increased their rates in 6-10 years.




