SSRIs
Do Antidepressants Work? Yes, No, and Yes Again!
The more depressed you are, the more likely you'll benefit from antidepressants.
Posted February 22, 2018 Reviewed by Abigail Fagan
Do antidepressants really work? This has been a controversial question ever since the 2008 publication of a research study by Dr. Irving Kirsch and his colleagues that concluded that there was “little evidence to support the prescription of antidepressant medication to any but the most severely depressed patients.”1 But now a new study, just published in The Lancet, indicates that yes, antidepressants do work for the treatment of depression after all.2
With seemingly different conclusions, as is often the case in scientific inquiry, should we just let the findings cancel each other out and believe what we want to believe? Of course not. Instead, as we try to make sense of the data, let’s look at both studies with an eye towards where they might differ and where they might actually support the same conclusion.
The 2008 study by Dr. Kirsch and colleagues was a meta-analysis of 35 randomized, controlled trials (RCTs) of antidepressants submitted to the Food and Drug Administration (FDA). FDA approval typically requires at least two “positive” studies that demonstrate the efficacy (in the case of depression, defined as at least a 50% reduction in symptoms) of a drug compared to placebo.
Knowing that FDA approved drugs have met this threshold of evidence, it would seem like a no-brainer to believe that antidepressants, true to their name, are actually antidepressants (though they can also help with other psychiatric conditions like anxiety disorders).
However, it’s important to understand that while two positive studies are required for FDA approval, there may be, and often are, other “negative” studies that fail to demonstrate that superiority over placebo. And in general, positive studies are published in journal articles and included in pharmaceutical advertisements, whereas negative studies are less likely to be accepted for journal publication and often aren’t even submitted. This “publication bias” contributes to the broad impression that medications are more effective than they really are,3 though it should be noted that this same overestimation has also been demonstrated for psychotherapy in the treatment of depression.4
In order to overcome this bias, Dr. Kirsch's meta-analysis included all of the studies, both positive and negative, for the six “new” antidepressants approved by the FDA between 1987 and 1999. With the mixed positive and negative results of those studies, they found that overall, antidepressant medications were no better than placebo for mild to moderate depression.
Although this finding was carried widely in the popular press at the time, it was often conflated with the conclusion that “there is no real antidepressant drug effect at all.” Indeed, a much-read New York Times Review of Books piece by Dr. Marcia Angell pulled that very quotation directly from Dr. Kirsch’s book The Emperor’s New Drugs: Exploding the Antidepressant Myth. Those eager to bash antidepressants have been running with this claim ever since.
As always though, the devil is in the details. Dr. Kirsch’s study didn’t so much show that antidepressants don’t work, but rather that placebos often work just as well when the person taking them is enrolled in a research study and has only mild to moderate depressive symptoms. This shouldn't be surprising when we remember, as I explained in a previous blog post called “The Healing Power of Placebos: Fact or Fiction?”, that placebos aren’t merely “sugar-pills” (in fact, they aren’t even sugar-pills at all).
In RCTs, placebos represent all of the interventions offered in a research study (e.g. psychiatric evaluation, supportive care, monetary compensation, etc.) besides the active medication, along with the power of the belief that one could be taking the active drug. In addition, subjects enrolled in clinical trials for depression are almost always outpatients with milder forms of depression, and it has been shown that placebo response in clinical trials increased substantially during the period of time between 1980 and 2000.5
So, what Kirsch’s study really showed was that for patients with mild and moderate depression, antidepressants didn’t add all that much to supportive interventions. A subsequent reanalysis of Kirsch’s data, using a different methodological threshold of “effect size” to determine statistical significance, agreed that antidepressants were no better than placebo for mild depression, but found that they were superior to placebo for moderate depression.6
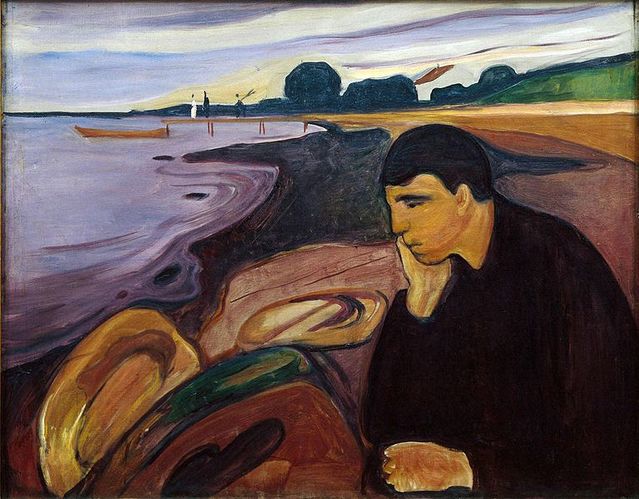
Notably, Dr. Kirsch’s study did conclude that antidepressants were most likely to work better than placebo for severe depression, supporting the related possibility that mild depression and severe major depression are two fundamentally different things. Major depression, or what used to be called melancholia, isn’t merely feeling depressed or down in the dumps in the setting of life events such as the end of a relationship, the death of a loved one, or the loss of a job. It’s a syndrome, or a constellation of co-occurring symptoms, that includes not just depressed mood, but “neurovegetative” features like insomnia, loss of appetite, feeling drained of energy, and the inability to enjoy the things that typically make us happy. For those with symptoms like these that persist despite supportive interventions, antidepressants are an integral part of treatment along with psychotherapy.
So, let’s move on to the new study published in The Lancet this week by Dr. Andrea Cipriani and colleagues. This meta-analysis was much larger in scope than Dr. Kirsch’s study, including 522 randomized, double-blind, placebo-controlled studies of 21 different antidepressants, including some not available here in the US, as well as two “old” antidepressants, the tricyclic drugs amitriptyline and clomipramine. Based on their analysis of pooled clinical trials, including both positive and negative trials submitted to the FDA, all 21 antidepressants were found to have superior efficacy in the treatment of depression compared to placebo.
Why the difference in conclusions between the studies by Dr. Kirsch and Dr. Cipriani? First, when it comes to meta-analysis, size matters. Compared to Dr. Kirsch’s study of only 6 medications and just over 5,000 patients, Dr. Cipriani’s study included over 100,000 patients such that it is the largest meta-analysis of antidepressant RCTs performed to date. It therefore represents the most comprehensive dataset upon which to base conclusions about antidepressant efficacy.
Second, it should be noted that the two studies by Dr. Kirsch and Dr. Cipriani are hardly the only meta-analyses that have ever examined antidepressant efficacy. Other studies, for example, have reinforced Dr. Kirsch’s conclusion that antidepressants are most effective compared to placebo when depression is more severe,7,8 while noting that it is placebo response, not antidepressant response, that varies and is lost as severity of depression increases.9
Unlike Dr. Kirsch’s study that intentionally examined differences in treatment response according to baseline depression severity, Dr. Cipriani’s study didn’t look at outcomes in this way, but rather found general antidepressant superiority across the pooled clinical trials for each of the 21 different antidepressants. It is possible that had the study stratified patients by depressive severity, it would have found similar results as that of Dr. Kirsch's meta-analysis.
For the inevitable naysayers tempted to dismiss studies based on claims that all researchers of psychiatric medications are pharmaceutical company shills, Dr. Cipriani’s work for this study was supported by the National Institute for Health Research with no declared compensation from the pharmaceutical industry. And unlike the findings of this current study, similar research by his research group has demonstrated no clear advantage for antidepressants in the treatment of children and adolescents with depression.10 And finally, one of his co-authors, Dr. John Ioannidis from Stanford University, has been a vocal critic of antidepressant efficacy in the past.11 So, this is hardly the work of researchers with a pro-medication agenda.
Looking beyond differences at the common findings across both studies, what can we take home from the research? Antidepressants don't work if you don't have depression. But if you do, they're more likely to work the more depressed you are in comparison to supportive care alone. Connecting this conclusion to other research findings, antidepressants may be overprescribed at the mild end of the depressive spectrum when patients are sad but don’t actually have major depression. For patients with severe depression, antidepressants are often underprescribed.
Antidepressants aren’t “happy pills,” have side effects that range from troubling to life-threatening, and shouldn’t be doled out like candy. But for patients struggling with major depression and melancholia, they can be lifesavers.
References
1. Kirsch I, Deacon BJ, Huedo-Medina TB, et al. Initial severity and antidepressant benefits: A meta-analysis of data submitted to the Food and Drug Administration. PLoS Medicine 2008; 5(2):e45.
2. Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. The Lancet 2018. online at: http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(17)32802-7/fulltext
3. Turner EH, Matthews AM, Linardatos E, et al. Selective publication of antidepressant trials and its influence on apparent efficacy. New England Journal of Medicine 2008; 358:252-260.
4. Driessen E, Hollon SD, Bockting CLH, et al. Does publication bias inflate the apparent efficacy of psychological treatment for major depressive disorder? A systematic review and meta-analysis of US National Institutes of Health-funded trials. PloS ONE 10(9):e0137864.
5. Walsh BT, Seidman SN, Sysko R, Gould M. Placebo response in studies of major depression: Variable, substantial, and growing. JAMA 2002; 287:1840-1847.
6. Vohringer PA, Ghaemi SN. Solving the antidepressant efficacy question: Effect sizes in major depressive disorder. Clinical Therapeutics 2011; 33:B49-B61.
7. Khan A, Leventhal R, Khan SR et al. Severity of depression and response to antidepressants and placebo: An analysis of the Food and Drug Administration database. Journal of Clinical Psychopharmacology 2002; 22:40-45.
8. Fournier JC, DeRubeis RJ, Hollon SD, et al. Antidepressant drug effects and depression severity: a patient level meta-analysis. JAMA 2010; 303:47-53.
9. Fountoulakis KN, Moller HJ. Antidepressant drugs and the response in the placebo group: The real problem lies in our understanding of the issue. Journal of Psychopharmacology 2012; 26:744-750.
10. Cipriani A, Zhou X, Del Giovane C, et al. Comparative efficacy and tolerability of antidepressants for major depressive disorder in children and adolescents: A network meta-analysis. The Lancet 2016; 388:881-890.
11. Ioannidis JPA. Effectiveness of antidepressants: An evidence-based myth constructed from a thousand randomized trials? Philosophy, Ethics, and Humanities in Medicine 2008; 3:14.




