Resilience
How to Identify an Individual Patient’s Resilience
The Resilience Scale detects a patient's positive and negative experiences.
Posted February 8, 2024 Reviewed by Gary Drevitch
Key points
- Scientific and humanistic medicine includes patients’ social experiences.
- Medicine falls short in addressing patients’ experiences and lacks proven methods to address social problems.
- The evidence-based Resilience Scale addresses individual patient’s experiences.
With rampant problems of loneliness since COVID-19 and the disturbed social lives of mass shooters, we’re hearing more and more that medicine and others must intervene on social issues that influence an individual patient's health and well-being. Not only a practical issue, this also is dictated by medicine’s systems-based scientific model: the biopsychosocial model. Unhappily, the latter has been fully implemented only at the biological (disease) level, but progress in systematically identifying an individual patient’s psychological features has occurred with the advent of evidence-based patient-centered interviewing.1 Sadly, there has been almost no success in addressing positive and negative social experiences that impact lifelong health outcomes.
Yet, plentiful population-level (epidemiological) data indicate the importance of understanding childhood adversities as well as positive experiences that enhance resilience and the youngster’s ability to learn to adapt. Now lacking, however, are validated interventions on a personalized basis for practitioners, organizations, and policymakers. This is in stark contrast to the evidence-based, individualized risk factors we have in, for example, cardiovascular disease, such as lipid levels, blood pressure readings, and exercise tests. To illustrate, elevated cholesterol in a young patient is a well-established risk factor for an adverse outcome (premature heart disease), but abuse and poverty, for example, have much less relationship in the individual child to adverse outcomes. Why? We also need to know what supportive factors may exist and how well the child learns to cope. To be certain, many individual risk factors are being explored, such as cortisol levels, telomere lengths, measures of executive function, and heart rate variability. But these are costly and labor intensive, and normative and predictive value research is inchoate.2
Encouragingly, however, a remarkable, long-term research project has developed a way to identify relevant social experiences in a given child and, in turn, to use this information to intervene at the clinician and organizational levels; I’ll summarize here, but extensive details can be found at the Alberta Family Wellness Initiative (AFWI). The Palix Foundation, a private Canadian foundation headed by Nancy Mannix, created the AFWI to improve the health outcomes and well-being of the children and families of Alberta, with a particular interest in mental health and addiction problems stemming from childhood adversity. The AFWI recognized two impediments to its goals: (1) there was no universal, evidence-based method to address an individual patient’s problematic and/or positive social experiences, and (2) clinicians, community organizers, and policymakers lacked information on how to address relevant experiences in a consistent, evidence-based way. Therefore, the research first identified a method and demonstrated its positive impact; it then developed a teaching method to train clinicians, organizers, and policymakers.
The Brain Story
The unique aspect of the AFWI approach, its various components dating to the early 2000s, is grounding its method and teaching in the science of the brain in a way that makes it accessible outside neuroscience to, for example, practitioners, social workers, and politicians. Toward this end, AFWI uses what they call the Brain Story. Developed by the National Scientific Council on the Developing Child, Harvard Center on the Developing Child, and the FrameWorks Institute, the Brain Story uses simple metaphors to communicate the science of brain development in an easily accessible manner. The AFWI shares the Brain Story through the Brain Story Certification Course—a free, online resource that shares knowledge about the science of brain development with families and professionals so that they may better understand how our earliest experiences can affect our long-term mental and physical health. Instruction in the Brain Story, however, is just the start.
The Resilience Scale
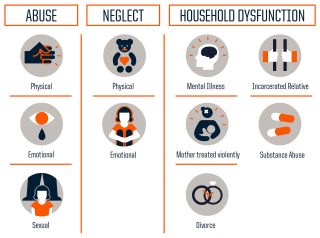
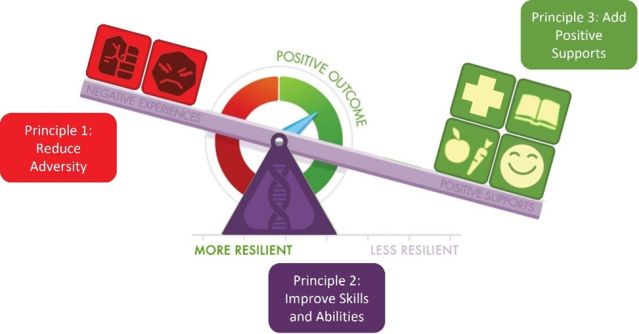
The next step teaches the various learners how to evaluate the balance of positive and negative experiences in a child’s life using the Resilience Scale developed by the National Scientific Council on the Developing Child. The Resilience Scale is a tool that exemplifies how resilience is the result of the interplay among our adverse experiences, our positive supports, and the functioning of our skills and abilities. A coding scheme developed by the Harvard Center on the Developing Child’s Frontiers of Innovation allows rigorous scientific evaluation of the scale. By applying this scale to the individual youngster, they generate a unique developmental profile that allows the patient and their family to better understand the child’s experiences. The Scale also allows them to direct care by identifying which area they would like to address. It also indicates where the clinician should intervene, where community organizers can help, and the areas needed to provide a comprehensive systems approach in any given community.
Here's what’s exciting, the details of which can be found at the Alberta Family Wellness Initiative: Investigators not only systematized a training approach, but they also evaluated and validated it to some extent. Learners (clinicians, organizers, politicians) first read three hypothetical individual case scenarios that contained details that could be mapped onto the Resilience Scale. Next, they coded elements within each scenario to construct that individual’s unique Resilience Scale. Respondents then explained to investigators why they coded items from the scenario as a source of adversity, a positive support, or as relating to the individual’s skills and abilities. The responses were then compared to gold standard ratings by the investigators. To date, 308 trainees have been evaluated, providing preliminary validation of the approach; many more studies are underway to further establish it. At the individual level, the Resilience Scale is also a tool for assessment and for tracking change over time. Ambitious future AFWI plans comprise working to integrate the Resilience Scale into current health system platforms, thus making it easier to access and apply. The Resilience Scale Training will soon be available as an online resource, but, in the meantime, it can be found at the website, Brains: Journey to Resilience.
At the organizational level, researchers found that the Harvard Center on the Developing Child’s Frontiers of Innovation coding scheme maps directly onto the Resilience Scale. This simple framework allows organizations to code programs and services according to what part of the Resilience Scale they target based on whether their primary objective is to reduce sources of adversity, add positive supports, or improve skills and abilities. Used in 11 organizations in Alberta, the team found very positive feedback suggesting the Resilience Scale can be successfully used as a tool for organizational change management. For the future, researchers seek to embed the Resilience Scale coding scheme into existing referral networks, allowing providers to make referrals according to the area of a client’s Resilience Scale that should be addressed; the updated referral network will also indicate whether consultants are trained in the Resilience Scale.
At a systems level, to achieve competency and active engagement from community leaders, two efforts to achieve this are (1) ensure that training in the Brain Story and Resilience Scale is widely available and successfully used, the idea being that, over time, various community leaders will be guided by this brain-based approach, and (2) facilitate "communities of practice" to bring together practitioners, policymakers, and organizers who are working with the same populations of patients, a community-driven initiative. This has been operationalized by one city signing a memorandum of understanding of the intention to apply this strategy and act as a pilot project to guide subsequent efforts. The Resilience Scale can be used to create systems integration and improve outcomes for individuals, families, and communities. In the future, the AFWI seeks to establish community mapping programs that depict health-related systems as a network of interconnected entities.
One reason AFWI research demonstrated successful learning of the teaching is that they developed a repeatable method, the prerequisite for systematic research. Furthermore, a standardized method means that those conducting training are teaching the same thing. Fully implemented, this allows a universal approach.
The work done by the Palix Foundation and the Alberta Family Wellness Initiative to operationalize an approach to understanding, tracking, and building an individual’s resilience pattern is groundbreaking. Their Resilience Scale offers a practical, evidence-based means for training practitioners, policymakers, and community organizers to address the social needs of individual patients at diagnostic and therapeutic levels.
References
1. Smith RC. Making the biopsychosocial model more scientific—its general and specific models. Soc Sci Med 2021;272:113568.
2. Shonkoff JP, Boyce WT, Bush NR, et al. Translating the Biology of Adversity and Resilience Into New Measures for Pediatric Practice. Pediatrics 2022;149(6). DOI: 10.1542/peds.2021-054493.




