Smoking
Why Are So Few Smokers Receiving a Life-Saving Test?
A simple test may reduce lung cancer deaths by 50 percent.
Posted May 20, 2019
Recent studies have demonstrated that only 2 percent of U.S. smokers who are eligible for lung cancer screening are undergoing the test. This poor rate is especially lamentable in view of a recent Japanese study demonstrating that screening can reduce lung cancer mortality by as much as 50 percent. Because lung cancer, which is diagnosed in over 230,000 Americans each year, is also the nation’s number-one cancer killer, tens of thousands of lives are being lost every year. Why are so few smokers getting the recommended screening?
The Test
The U.S. Preventive Services Task Force recommends annual low-dose CT screening in adults between 55 and 80 years of age who have smoked the equivalent of a pack a day for 30 years and who currently smoke or have smoked in the past 15 years. The noninvasive test, which takes less than a minute, produces CT scan images of the lungs. Radiologists inspect the images for small cancers. Finding small lesions is important because larger lung cancers that have already spread have a poor prognosis, but small ones can often be removed before they spread, resulting in a cure.
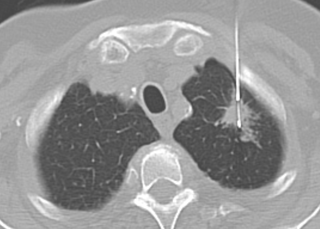
When most smokers undergo screening, there are no findings suspicious for cancer, and patients are advised to return for a repeat scan the next year. In other cases, a small lesion called a nodule is detected, in which case a follow-up CT scan may be obtained in a few months to see if it is growing. In other cases, a larger lesion is discovered, in which case, a biopsy may be necessary, or another scan called a PET scan may be performed to see if the lesion represents cancer.
Low Screening Rates
There are many possible explanations for the fact that so few patients are undergoing screening. For one, many physicians are not discussing screening with eligible patients. In one study, such conversations took place between physicians and patients only 4 percent of the time. Pressures to speed up medical practice have made many patient visits so short that there is little time to talk about screening exams.
Another factor may be discomfort among patients and physicians about discussing a deadly disease. In many cases, patients are seeing their doctors because they are already sick or under treatment for another disease. Under such circumstances, raising the specter of lung cancer may seem like adding insult to injury.
Another factor may be the cost of screening. Yet Medicare and many private insurers cover the cost of the screening test for eligible patients, at least up to age 77. Of course, some patients may face copayments and deductibles, and others may lack insurance altogether.
Another issue for some patients is the difficulty of getting the test. Patients in large cities are likely to live or work near a testing center, but many others live in relatively sparsely populated regions of the country, sometimes hundreds of miles from such facilities.
Other patients may decline to get the test because they have heard that CT scans involve radiation exposure. It is true that every CT scan uses x-rays, but the screening scans are called “low dose” for a reason—they involve small radiation exposures, and the benefits of screening in detecting cancers early are thought to vastly outweigh the risk of causing cancer. The same goes for the risks of any subsequent testing that might be necessary, such as a biopsy or PET scan.
A final concern for some is the risk of false-positive findings; in some cases, a finding suspicious for cancer turns out to be something else. The additional tests needed to determine if a lesion represents cancer impose risks and costs of their own, including the anxiety associated with an abnormal test result, which some patients may prefer to avoid. On the other hand, discovering that a lesion is not cancerous can be quite a relief.
Moving Forward
Of course, the best means of reducing lung cancer mortality is for patients to avoid smoking entirely, and for those who do smoke, to quit as soon as possible. Nevertheless, about 9 million Americans qualify as high risk for lung cancer, and low-dose CT screening represents the best means we have of preventing them from dying of lung cancer. If we are to avoid such deaths, we need to better understand and address the psychological considerations that are preventing patients from getting the test.


