Health
The Next Frontier of Human Health: the Metabolome
Our genes are less important than the output of genetic programming.
Posted December 30, 2019 Reviewed by Matt Huston
Headlines for science often trumpet new findings in genetics, purporting to be the key to understanding health and disease. The newest sexy (and, to be fair, very exciting) genetic story is about CRISPR, a type of genetic manipulation that can splice and replace genes in a precise program.
But genes are only the first-order programming for human development and maintenance of tissues. Genes have to be turned on to be used, the proteins from the direction of the genetic code have to be spliced and transported to the right places at the right times. A lot can go on between the genetic code and the final product that has huge effects on health and disease.
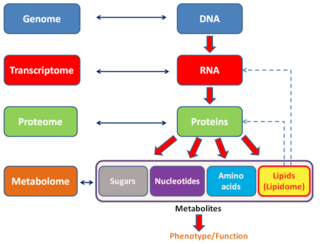
This is where the metabolome comes in. Your cells make everything from amino acids to waste products to fatty acids and DNA. While the genetic code is the initial programming, the metabolome is the eventual output of all that programming. The metabolome tells us how the genetic code is interacting with the environment, and the more we know about the metabolome, the more we can understand how the environment makes its impact on our health.
The study of metabolomics is old (one of the earliest stories you learn in medical school is how doctors in days of yore would diagnose diabetes by tasting urine and finding it sweet). However, the systematic, full organism study of metabolomics is quite new, mostly because we never had the computing power to deal with all the data until recently. Nowadays there are large databases of metabolites that can be accessed for free, or for a price, depending on your needs.
What does this have to do with psychiatry? It’s early days yet but there are some exciting things going on with respect to the metabolome and mental illness. I’m not even talking about the metabolome of our microbiome, discussed here, but rather the output of our own cells. Researchers are studying human brains to try to figure out the basic pathology underlying schizophrenia. While we don’t understand everything by any means, we know that a basic step where things go wrong is in development of synapses, particularly what we call the “excitatory” synapses that are the “on” buttons of neurons.
Excitatory synapses are tightly coupled to energy flow, which makes sense. They use a lot of energy. This means the generation of energy and the proper disposal of waste products are very essential to the proper function of excitatory synapses. In studying human brains, researchers found that people with schizophrenia tended to have more acidic brains in certain areas than normal controls, which suggests there is something wrong with the metabolism in that area of the brain. You see, part of a smoothly functioning brain metabolism is shuttling an acid, lactate, around to the right places. If the lactate isn’t moving around the way it should, the pH can drop. Why would this be?
Well, researchers went further and found out that certain enzymes important to metabolism were not functioning correctly in these brain samples from patients with schizophrenia. Using this sort of data, figuring out which enzymes were faulty in this area of the brain by measuring metabolic output, pH, etc (all part of the metabolome of that area of the brain), researchers can backtrack and figure out what pharmaceuticals can ameliorate some of these deficits. Not only known pharmaceuticals that we might already use to treat mental illness, but also orphan drugs—developed for one specific purpose and then abandoned—as well as medicines that are in use for entirely different things to see if they might be useful for schizophrenia. In order to do this, researchers consult a huge database called LINCS, which has the metabolomic signatures of 1.5 million pharmaceuticals on file.
The same kind of reasoning and cellular measurements of metabolome can be used not just for pharmaceuticals (new and old), but also for other environmental treatments, such as exercise or a ketogenic diet. In the schzophrenia issue, a ketogenic (very low carbohydrate) diet could theoretically bypass some of the metabolic problems found in the brains of people with schizophrenia, thus theoretically improving symptoms (and if used early enough, it could have a role in prevention). There are case studies in the literature for this treatment, but controlled trials have only just begun.
Big data combined with microscopic-level insight and clinical wisdom could help us cure or prevent many diseases and improve worldwide health. Study of the metabolome is the biggest and possibly the most fruitful frontier of human medicine.
Copyright Emily Deans MD


