Paranoia is not simply synonymous with fear. It's yet another psychiatric term misrepresented and misunderstood by society at large that seeps into clinical work. More than once I've had to remind a student or supervisee that someone fearing the worst, like in anxiety, does not qualify as paranoia.

Though I just bashed pop culture for misrepresenting paranoia, there's a popular Vietnam-era song I've used to help people understand it.
“Paranoia strikes deep…” goes the Buffalo Springfield song "For What It’s Worth." The 1966 hit is interesting not only because it’s a song in which the title doesn’t appear in the lyrics, but it gives such an accurate description of the experience of paranoia.
Paranoia, defined
The word paranoia is derived from the Greek, “para,” meaning beyond/outside, and “noos,” meaning the mind. Translated, we arrive at “out of their [right] mind,” or “a mind distracted.” Like most psychological phenomena, paranoia exists on a continuum. It's familiar to most of us, though it was probably fleeting, situational, and an appropriate response.
I felt it intensely once, while camped out alone in a remote mountain campground in Oregon’s Cascades. Few were around and late in the day a couple pulling a camper arrived. The man came over and made small talk, though asked a lot of questions, some seemingly to probe for if I was alone. Becoming wary, I kept my eye on them and I didn't sleep; at about 1 in the morning he exited the camper and muddled about their area. The bad vibe became stranger to me, and, heart in my throat, I disassembled camp in five minutes and fled. Given the circumstance, it was an adaptive psychological experience. I was alone, and their strange actions led me to perceive a threat, initiating the survival mechanism of fleeing. But what about people whose lives consist of regularly feeling something like my experience, even in the absence of obvious threat?
It doesn't just happen. “…into your life it will creep,” continues the tune. People who are pathologically paranoid didn’t just have an experience like mine, and it stuck. Paranoia is often of an insidious onset, whether it is related to PTSD, someone’s personality, or in delusional psychotic states. It could be weeks or months of evolution. Learning of the person’s background, we often discover that paranoid ideas indeed creep into one’s thought process until it fully colors their general view of things.
Paranoia's three manifestations
People with PTSD often suffer from hypervigilance; they're acutely aware of their surroundings and ready to fight or flee. For some, especially war veterans, hypervigilance can be so severe as to take on a paranoid flavor. I’m reminded of Vietnam veterans who were chronically ambushed and how my uncle described, like the lyric, “It starts when you’re always afraid…”
Fear, a natural survival mechanism, becomes so honed from being chronically “on" that it takes on a life of its own, eventually toppling into paranoia. Even rustling breezes can put one on edge: “Stop! ... What’s that sound?” To my uncle, everything seemed a sign of impending ambush. Given the acute survival situation, this again is adaptive, albeit disturbing.
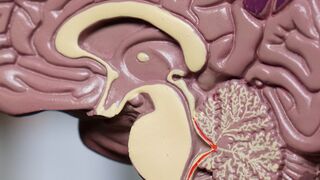
The problem is, for people who have been exposed to chronic, acute survival scenarios, they can’t just shut it off when the situation is over. Their limbic system, the brain's survival center, has learned being "on" is now essential to exist. Interestingly, under such chronic stress, the amygdala, an almond-sized-and-shaped structure (amygdala being Greek for almond) that is the seat of fear in our limbic system, actually expands abnormally. Coming home, the soldier remains stuck in a state of hypervigilance and is distractingly aware of their environment. “… look what’s [maybe about to be] going down."
There's emerging evidence that an enlarged amygdala can be reduced, and with it, symptom acuity, especially via mindfulness practice. Whether a shrinking amygdala is wholly responsible for decreased symptoms remains to be seen. Regardless, the good news remains that we know mindfulness practice, grounding, and relaxation skills can lower the amperage and the person can be coached into being less on edge.
Paranoid Personality Disorder
Another stage for persistent paranoia is someone’s personality. Personality has a lot to do with how we interact with others. When a person’s interactional style is informed by acute suspiciousness of the motives and intentions of others, there's like a paranoid personality at hand. It's believed that Watergate was spurred by Richard Nixon’s paranoid personality characteristics, exemplifying just how pervasive such suspiciousness can be. Such individuals are prone to global, distorted thinking like the following:
- Anyone wanting to get close to them is going to try to take advantage
- Reading compliments as being buttered up for something
- Perceiving casual comments as slights (e.g., Coworker: “Nice tie, Adam!” Adam: [inner voice] “What’s that supposed to mean?!)
Many with paranoid personality have an early background of abuse and learned to be mistrustful so as not to get hurt. Even sincere compliments are shunned; “Compliments can be someone’s way of trying to get close to me. I don’t swallow it. Back off!” Thus, they retain an aloof aura, in order to keep others at a distance.
Psychotic Disorders
Lastly, there's delusional paranoia as seen in psychotic disorders like schizophrenia or mood disorders with psychotic features. A delusion is a fixed, false belief that is held with conviction. You can’t talk someone out of a delusion. It's their reality as much as the rest of us know the sky is blue. Paranoid delusions tend to take on themes of conspiracy, jealousy, and persecution. Paranoia expert Ronald Siegel, Ph.D., in his landmark book Whispers: The Voices of Paranoia, succinctly describes an example of a paranoid delusional experience:
You draw the attention of the First Lady. She falls in love with you. Of course, she cannot make a definite avowal of her love, but she shows it in many silent, indirect ways. Her husband learns of her secret desires and lashes out at you. He sends in the FBI, the Secret Service, then the Mafia. You fight back with lawsuits against the government and the phone company…

Clearly, this is the kind of “out of their mind” state the ancient Greeks were describing; there's no question to him—everyone is a spy or enemy. Having interacted with people suffering like this, I’ve been amazed at how others can become drawn into their reality, they discuss it so convincingly. Amazingly, reducing the neurochemical dopamine can deconstruct such thinking, and is what antipsychotic medications like Haldol, Zyprexa, and Abilify accomplish.
Treatment implications
- PTSD patients tend to welcome grounding techniques to learn to quell their amygdalar hypersensitivity.
- Paranoid personalities rarely enter treatment given their extreme, global suspiciousness. However, therapists may recognize a patient is struggling with someone with paranoid personality and must help them navigate having them in their lives. Psychiatrist Stuart Yudofsky's book Fatal Flaws has a section on evaluating and managing this condition.
- A patient with delusional paranoia, given the excessive dopaminergic activity, will likely require a referral to psychiatry or inpatient care before they can be worked with in psychotherapy.
Paranoia is an incredibly pervasive situation. It's important to not only recognize the condition, but to quickly distinguish amongst its three faces in order to provide the most sound intervention.
This post also appeared on Psych Central.
References
Siegel, Ronald K. (1994). Whispers: the voices of paranoia. Simon & Schuster.
Yudofsy, Stuart. (2005). Fatal flaws: Navigating destructive relationships with people with disorders of personality and character. American Psychiatric Publishing, Inc.




