Persuasion
The "Electrochemical Persuasion" of Neuromodulation
Was the treatment of obesity ever "brainless?"
Posted August 13, 2016

In the totalitarian future of the novel We, written in the 1920s by Russian novelist Yevgeny Zamyatin, the Benefactor rules One State; there is no privacy, and people, known only by numbers, live in glass houses. The main character D-503, a mathematician, commits the sin of falling in love. He is suffering from the “illness of imagination,” whose cure is “exclusively a matter of surgery” i.e., "a special brain operation invented to excise imagination forever."
Likewise, in George Orwell’s 1984, Winston Smith’s torturer says, “We control matter because we control the mind.” He adds, “Power is in tearing human minds to pieces and putting them together again…we burn all evil and all illusion out of him…we make the brain perfect…” As a result of his torture, Winston believes “as though a piece had been taken out of his brain.” Ironically, in the language of Newspeak, “there was indeed no word for Science.”
These two dystopian novels tap into the feelings most people have that there is something particularly disturbing and even creepy about attempts at changing behavior through manipulation of the brain. But this is not just science fiction: it was not so many years ago that physicians attempted to modify a patient’s behavior with the psychosurgical procedure of frontal lobotomies, and many remember the vivid scene in the film One Flew Over the Cuckoo’s Nest when the Jack Nicholson character received ECT for his recalcitrant behavior.
Is there a place for a kind of behavior control, as it were, through either direct or indirect stimulation of the brain in the treatment of obesity and eating disorders? Some researchers think so. After all, these disorders are difficult to treat and our current treatments, including psychological ones, have “only limited efficacy.” (Schmidt and Campbell, European Eating Disorders Review, 2013) Researchers are now turning to the “emerging neurotechnologies” of both invasive and non-invasive brain stimulation. In other words, treatment is definitely not “brainless.” (Schmidt and Campbell, 2013; McClelland et al, 2013, (European Eating Disorders Review)
Back in 2005, Spiegel et al (Nature Neuroscience) wrote an article “Obesity on the Brain.” These researchers proposed to focus on “neurobiology, behavior, and obesity” in developing their strategic plan for obesity research in their attempt to understand why some people overeat and remain sedentary. They emphasized that imaging studies, such as MRI and positron emission tomography “thus becomes the cornerstone of efforts to understand the biology of human eating behavior.”
Along those lines, Alonso-Alonso and Pascual-Leone wrote (JAMA, 2007), “The Right Brain Hypothesis for Obesity.” These authors suggest that the right prefrontal cortex is “preferentially” involved in decision-making and question whether deficits in this area of the brain “may contribute to the inability of some obese patients to commit to weight loss interventions long term…” as well as to their failure to consider the adverse consequences of their “obesogenic” behaviors. This article sparked a lively debate in which Bachman et al (JAMA, 2007) wrote, “Before adding the stigma of 'brain damaged' to the high physical and social burden obese persons already bear, we would like to see more compelling data to support the conclusion.” Pascual-Leone et al defended their position: “Finding a pattern of brain activity associated with a given behavior or disorder should not be taken as revealing ‘brain damage,’” but rather could lead to brain “targeted therapies.” (JAMA, 2007)
The situation, though, is complex, and “theories of aberrant neural responses” for both obesity and eating disorders appear to conflict with each other: both increased and decreased responsivity to the reward circuit has been found. (Berger and Berner, Physiology & Behavior, 2014) Furthermore, though there are two major aspects of control of food intake—homeostatic (eating for survival, i.e., hypothalamic, reflexive) and hedonic (i.e., eating for pleasure, i.e., cognitively reward-based, reflective), the “degree to which homeostasis and hedonic systems interact to influence intake has yet to be fully understood.” (Berger and Berner, 2014)
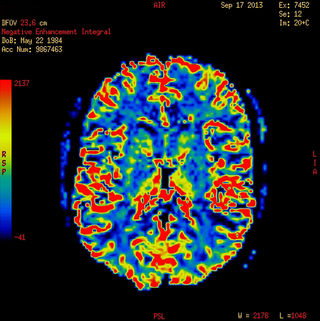
Satel and Lilienfeld, in their excellent 2013 book Brainwashed, raise the question of whether “neurodeterminism” is “poised to become the next grand narrative of human behavior.” They write that for many, “brain-based explanations appear to be granted a kind of inherent superiority over all other ways of accounting for human behavior”—what these authors call “neurocentrism,” and they call the pictures from MRIs “color-drenched brains.”
McCabe and Castel (Cognition, 2008), in their study, “Seeing is Believing…” demonstrate Satel’s and Lilienfeld’s argument. They explored how images of the brain, because they appeal to people’s need for “reductionistic explanations of cognitive phenomena” have a “particularly persuasive influence” and artificially lend a “great deal of scientific credibility:” those studies that incorporated brain images (rather than bar graphs or no images) became more scientifically credible to their subjects even when there were obvious errors in the data.
Likewise, Weinberger and Radulescu (Am. J Psychiatry, 2016) assert that findings that may seem “neurobiologically meaningful” may, in fact, represent, “artifacts or epiphenomena of dubious value.” These authors emphasize, for example, that MRIs are “not a direct measure of brain structure—an MRI is a “physical-chemical measure” and as such, many things (e.g. body weight, medications, alcohol use, nicotine use, exercise, hydration, pain, etc.) can affect variations in MRI signals and anatomical measurements. Furthermore, even head motion can be a “corrupting influence.” The main readout of an MRI is the blood-oxygen-level-dependent (BOLD) response that is only a “proxy used to indicate activity.” (Berger and Berner, 2014)

An article that highlights the potential for false positives in functional neuroimaging reads like a classic Monty Python skit. Bennett and his colleagues (Journal of Serendipitous and Unexpected Results, 2010) invited a mature dead Atlantic salmon (Monty Python might have used a dead parrot) to participate in an fMRI scan. There was no mention of whether consent was obtained but a “mirror directly above the head coil allowed the salmon to observe the experimental stimuli” and foam padding prevented excessive movement “but proved to be largely unnecessary as subject motion was exceptionally low.” The salmon “was asked to determine which emotion the individual in the photo must have been experiencing.” What the researchers found is that certain areas of the dead salmon’s brain actually lit up on fMRI—clearly a false positive. (We do not know, of course, whether a repeat experiment with a dead wild-caught Alaskan salmon would yield similar results.) Nevertheless, the authors confidently recommend continued fine-tuning of fMRI technology.
Given these caveats, what is neuromodulation? It is a technique, intended to change behavior, by targeting areas of the brain, (sometimes specific areas such as the dorsolateral prefrontal cortex, amygdala, or nucleus accumbens), either non-invasively or invasively, by various means. Parpura et al (Journal of Neurochemistry, 2013) explain that the “brain operates through complex interactions in the flow of information and signal processing within neural networks” and the “wiring” of these networks can sometimes “go rogue in various pathological states.” Neuromodulation, they note, “attempts to correct such faulty nets.” They describe its potential effects as “electrochemical persuasion.”

Neuromodulation procedures can be used either to stimulate or inhibit neural activity via different parameters such as frequency, duration, intensity, number of sessions and stimulation sites. (McClelland et al, European Eating Disorders Review, 2013) Val-Laillet et al (NeuroImage: Clinical, 2015) reviewed the two most common non-invasive neuromodulation techniques---transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS), as well as the two more invasive procedures--deep brain stimulation (DBS) and vagal nerve stimulation (VNS). Most studies involving either tDCS or TMS evaluate effects on food craving, subjective appetite, and food intake, including more recently, binge-eating. (Burgess et al, International Journal of Eating Disorders, 2016.) In this study, the researchers suggest that those people with the “cognitive mindset” to restrict caloric consumption may be particularly primed to respond to tDCS.
Val-Laillet et al (2015) note that the specifics of neuromodulation, including the most efficacious protocols “remain to be defined.” Furthermore, there is variability among the reactions of patients, including that sham procedures can evoke placebo responses. The techniques are not necessarily “ready for prime time.” For example, Gluck et al (Obesity, 2015) studied transcranial direct current stimulation (tDCS) administered to the dorsolateral prefrontal cortex of their subjects to assess caloric intake and potential for weight loss. They note that some current “does penetrate the brain” when they applied low amplitude direct currents with electrodes placed on the scalp: with cathode stimulation, nerves are less excitable and less likely to fire while anode stimulation increases their excitability and makes them more likely to fire. Unfortunately, in the first arm of their research, the anode and cathode leads had been inadvertently reversed, and the study had to be halted.
In general, though, Val-Laillet et al (NeuroImage: Clinical, 2015) note side effects with the non-invasive types are usually mild and can include neck pain, headache, tingling, itching, but the “most worrisome” is the induction of a seizure. They emphasize, though, “the current state of the science is far from being conclusive” in “the possibility of manipulating the human brain.”
McClelland et al (2013) reviewed 60 human and animal studies involving the four available (two non-invasive and two invasive) neuromodulation techniques: research indicates that neuromodulation has the potential for altering food intake, body weight, and disordered eating (e.g. as found in those with anorexia, bulimia or those who have strong food cravings.)
Studies from lesions have implicated three potential brain targets associated with increased food intake for consideration for the surgically invasive technique of deep brain stimulation (DBS): the lateral hypothalamus (appetite regulation), ventromedial hypothalamus (often considered the “satiety center” of the brain), and the nucleus accumbens (value of food, regardless of appetite.) (Kumar et al, Annals of Neuroscience, 2015) With DBS brain surgery, complications can be significant and include stroke.
The other invasive procedure is the newly FDA-approved vBloc, a reversible vagal nerve blockade that is far less invasive than bariatric surgery. The ReCharge Trial is ongoing (though many of those involved have conflicts of interest in that they have an affiliation with the manufacturer of this device.) To date, this therapy resulted in significantly greater weight loss than sham surgery, though those in the sham control group lost more weight than expected (Ikramuddin et al, JAMA 2014; Morton et al, Obesity Surgery, 2016) It is described as “a device that controls hunger and feelings of fullness by targeting the nerve pathway between the brain and the stomach.” Side effects include nausea, pain at the implant site, heartburn, vomiting and surgical complications.
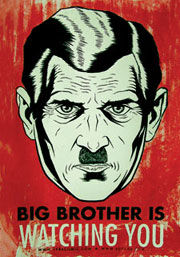
Both Val-Laillet et al (2015) Ho et al (Cureus, 2015) raise the bioethical issues involved in neuromodulation, as a “behavior-altering treatment.” For example, Ho et al question whether manipulating the rewarding aspect of food intake may have unforeseen consequences on a person’s ability to experience other pleasures. Clearly that was the intent in the “Big Brother” society of 1984.
Bottom line: Neuromodulation remains poorly understood, whether it involves “depth electrodes (i.e. DBS), arrays of microelectrodes penetrating the brain cortex, or cortical surface electrodes placed outside or inside the dura.” (Parpura et al 2013) These researchers emphasize that these techniques as practiced currently are “all insultingly inelegant for interacting with such a marvelous structure as the nervous system.”




