Vagus Nerve
Vagus Nerve Stimulation via the Outer Ear Takes Center Stage
Non-invasive vagus nerve stimulation reduces fight-or-flight stress responses.
Posted July 30, 2019 Reviewed by Abigail Fagan
The vagus nerve is called the "wandering nerve" because it's the longest nerve in the human body and travels from the base of the brain up into the ears and down into the lower intestines. In recent months, non-invasive vagus nerve stimulation (VNS) devices that do not require a surgical implant—but can reach the auricular branch of the vagus nerve that extends to the outer ear—have been making headlines.
Vagus nerve stimulation via the external ear using electronic devices has been shown to increase the "relaxation response" of the parasympathetic nervous system and reduce fight-or-flight stress responses driven by the sympathetic nervous system.
Earlier this year, I reported on a pioneering study (Addorisio et al., 2019) which found that using one of these electrical vagus nerve stimulation devices—that is applied to a specific region of the external ear by a technician—activated the parasympathetic system in ways that reduced inflammation. (See, "Vagus Nerve Stimulation Dramatically Reduces Inflammation.")
You can see how this vibrotactile device is applied to the external ear in the images below:

Today, a new study (Bretherton et al., 2019) from the University of Leeds reports that self-administered non-invasive transcutaneous vagus nerve stimulation (tVNS) via the outer ear—performed for 15 minutes daily for two weeks at home—boosted "rest and digest" parasympathetic activity and reduced "fight or flight" sympathetic activity in a cohort of adults 55+ years old.

This paper, "Effects of Transcutaneous Vagus Nerve Stimulation in Individuals Aged 55 Years or Above: Potential Benefits of Daily Stimulation," was published July 30 in the journal Aging.
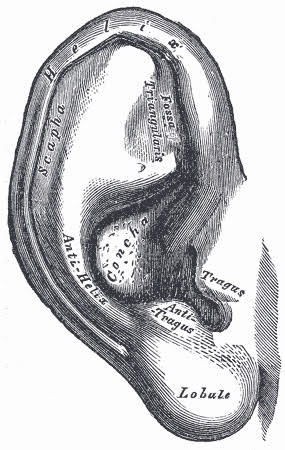
Previous research (Deuchars et al., 2017) by this University of Leeds group found that tVNS via the external ear improved autonomic function in healthy young participants. For their follow-up study (2019), the same tVNS technique was used. This non-invasive vagus nerve stimulation device has electrodes which are attached to the tragus section of the outer ear; the stimulating current is administered using a transcutaneous electrical nerve stimulation (TENS) machine.
According to the researchers, as we age, the sympathetic branch of the autonomic nervous system starts to dominate; this autonomic imbalance reduces optimal bodily functions and makes us more susceptible to illness as we get older. The good news: Their research suggests that stimulating the vagus nerve using a tVNS electrical device attached to the tragus region of the outer ear helps to rebalance the autonomic nervous system and may slow the adverse effects of aging in people over age 55.
In the paper's conclusion, Bretherton and coauthors sum up the significance of their findings on tVNS in older adults:
"For the first time, we have shown that age-related autonomic, quality of life, mood and sleep changes may be improved with transcutaneous vagus nerve stimulation administered [for 15 minutes] every day for two weeks. Importantly, the findings point to the influence of initial values in determining magnitude and direction of change following tVNS: high initial sympathetic prevalence, tension, depression, anger and confusion and low energy and sleep quality were associated with greater improvements. With further work, it may, therefore, be possible to identify which individuals will most benefit from daily tVNS in terms of their autonomic function and overall wellbeing."
"We believe these results are just the tip of the iceberg. We are excited to investigate further into the effects and potential long-term benefits of daily ear stimulation [of the vagus nerve], as we have seen a great response to the treatment so far," lead author Beatrice Bretherton, from the School of Biomedical Sciences at the University of Leeds said in a news release.
This recent three-part study (2019) by Bretherton et al. shows promise, but also has some limitations. The study's shortcomings include a small cohort of participants, the lack of control groups or a "sham" device for every arm of the study, and the possibility of "placebo effect" influencing the results. The authors acknowledge these limitations and offer some advice for next steps regarding tVNS research: "Future studies should also carefully consider their study design, especially with respect to control groups. This future work should also explore the extent to which the changes in the self-report measures were due to tVNS, a placebo effect, or a participant bias."
How Does Experimental tVNS via the Outer Ear Fit into a Timeline of FDA-Approved Ways to Stimulate the Vagus Nerve?
Decades ago, traditional implanted vagus nerve stimulation devices (like the VNS device in the illustration below) were FDA approved for the treatment of epilepsy. In 2005, implanted VNS devices were also approved for treating major depressive disorder and "treatment-resistant depression" in patients age 12 and older.

A recent "Review of vagus nerve stimulation as a therapeutic intervention," (Johnson & Wilson, 2018) concluded, "VNS has been proven to be a useful treatment across a number of domains and has been used effectively to treat epilepsy and depression in adults. There is accumulating evidence to suggest that it can be used to help quell inflammation in a number of other autonomic or inflammatory disorders, which would make it useful for a wider range of pediatric patients as well."
Last year, a hand-held VNS device called "GammaCore" (which is applied to the neck and pulses an electrical current through the skin to stimulate the vagus nerve) got FDA clearance to treat the pain associated with migraine headaches in adult patients. (See, "Non-Invasive Vagus Nerve Stimulation May Relieve Migraines.")
Note: There is also a wide range of technology-free ways to stimulate the vagus nerve, boost parasympathetic activity, improve vagal tone, and increase heart rate variability (HRV) that do not require any gadgets or electrical stimulation.
References
Beatrice Bretherton, Lucy Atkinson, Aaron Murray, Jennifer Clancy, Susan Deuchars, Jim Deuchars. “Effects of Transcutaneous Vagus Nerve Stimulation in Individuals Aged 55 Years or Above: Potential Benefits of Daily Stimulation.” Aging (First published: July 30, 2019) DOI: 10.18632/aging.102074
Susan A. Deuchars, Varinder K. Lall, Jennifer Clancy, Mohd Mahadi, Aaron Murray, Lucy Peers, Jim Deuchars. "Mechanisms Underpinning Sympathetic Nervous Activity and Its Modulation Using Transcutaneous Vagus Nerve Stimulation." Experimental Physiology (First published: November 11, 2017) DOI: 10.1113/EP086433
Meghan E. Addorisio, Gavin H. Imperato, Alex F. de Vos, Steve Fort, Richard S. Goldstein, Valentin A. Pavlov, Tom van der Poll, Huan Yang, Betty Diamond, Kevin J. Tracey, and Sangeeta S. Chavan. "Investigational Treatment of Rheumatoid Arthritis with a Vibrotactile Device Applied to the External Ear." Bioelectronic Medicine (First published: April 17, 2019) DOI: 10.1186/s42234-019-0020-4




