Depression
How Should We Treat "Contested" Illnesses?
The relationship between contested illnesses and psychiatric illnesses.
Posted June 8, 2019 Reviewed by Devon Frye
A friend recently visited his doctor because of a bad cough that had lasted a few weeks. He didn’t otherwise feel sick and worried he might have lung cancer or some other life-threatening disease.
When all the test results were in, his doctor happily said, “I can’t find anything at all wrong with you. Maybe just allergies. Nothing to worry about.”
The friend was ecstatic to hear this news, even though it meant he had no further information about what was causing his cough or any treatment for it. To know he didn’t have cancer was enough to make him happy.
The above scenario is more common than we sometimes think. Often, medical science, despite all the incredible things it can now do, cannot find any explanation for symptoms that we have and we have to accept vague suggestions for the cause of our problems, like too much stress or allergies.
For people with what are called “contested illnesses,” however, that uncertainty can become unbearable. As months and months of pain and suffering persist unabated, the need to find answers mounts. Those answers, many insist, should not be “there is nothing wrong with you” or “it’s just depression.”
Contested Illnesses Become Contentious
Contested illnesses include conditions like chronic fatigue syndrome (CFS, also called myalgic encephalomyelitis or ME), fibromyalgia, multiple chemical sensitivities, and chronic Lyme disease. According to David Scales, an internist, sociologist, and Critica Chief Medical Officer, “Contested illnesses have uncertain causes, unclear treatments, and disputed medical, legal and cultural definitions."
These conditions are called “contested” because some people, including physicians and scientists, dispute their existence. This has led to the formation of patient advocacy organizations like Solve ME/CFS, the National Fibromyalgia and Chronic Pain Association, and the International Lyme and Associated Disease Society. Each of these organizations provides information about their respective illnesses, lobby for increased research funding, and advocate for acceptance of the illnesses as distinct biological entities.
In some instances, organized medical groups have clashed with people suffering with contested illnesses. In 2017, for example, a group of 28 people sued the Infectious Disease Society of America (IDSA), claiming that its guidelines for treatment of Lyme disease leads to denial of coverage for more than a month of antibiotics. The IDSA says there is no evidence that more than 30 days of antibiotics is either safe or effective for treating symptoms after acute infection with the organism that causes Lyme disease, but people with such symptoms believe that longer courses of antibiotics are necessary. The controversy can sometimes appear quite contentious.
"It’s All in Your Head"
One of the things that many people with contested illnesses dislike is being told that their symptoms stem from an underlying psychiatric disorder. Indeed, they say, an incorrect diagnosis of depression is frequently given to people with CFS, fibromyalgia, and chronic Lyme disease.
It is not that people with contested illnesses are fabricating their symptoms. The physical pain they feel is real. It is the root cause that is in dispute. To people with contested illnesses, being told they are suffering with depression means it is “all just in my head.” As one patient who subsequently received a diagnosis of chronic Lyme disease put it: “Over and over I met with doctors who appeared relieved to find there was nothing wrong with me besides a misfiring brain. I was seen as overreacting to symptoms of depression due to my anxiety, even by those closest to me."
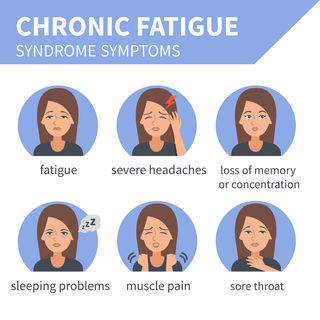
It is unsurprising that depression is often the diagnosis given to people with contested illnesses for several reasons. First, the diagnosis of depression is based on symptoms reported by the patient and observations of the patient’s behavior and mood made by significant others and clinicians. The symptoms prominently include depressed mood and loss of interest in usual activities, but also include physical symptoms like fatigue, insomnia, loss of energy, trouble concentrating, and headaches and other types of pain. Many of these symptoms show up in the symptom lists for the contested illnesses.
Second, although in most instances there are no FDA-approved medications for contested illnesses, antidepressants and various psychotherapies are among the interventions frequently recommended. For fibromyalgia, there are three FDA-approved drugs, two of which are antidepressants (duloxetine and milnacipran) and the third an anti-seizure medication (pregabalin). But the fact that medications for depression work for contested illnesses does not, of course, prove that contested illnesses are really part of or caused by depression. Although epidemiological studies show that patients with contested illnesses have high rates of psychiatric illnesses, including depression and anxiety disorders, those studies cannot tell us whether psychiatric problems cause the contested illnesses, the other way around, or both. We know that chronic pain is itself a risk factor for depression and high rates of depression are seen in most medical illnesses, like diabetes, heart disease, and cancer.
Diagnosing Depression May Be Seen as Insulting
These links between contested illnesses and depression do not, then, establish that depression is the underlying cause of any of them. Like contested illnesses, we do not have a definitive biological basis for depression, nor do we have objective tests that make diagnoses secure for any of these conditions. So trying to ascribe all cases of CFS, fibromyalgia, chronic Lyme, or multiple chemical sensitivity to depression is obviously not based on any clearly understood biology.
What is concerning, however, is the notion that suggesting something might be a psychiatric illness or that a person with chronic pain can also suffer from depression is interpreted as akin to dismissing the patient as a faker, someone who isn’t really sick. For example, an article in Slate states that, “There’s actually ample evidence against the theories that [chronic Lyme disease] is all in one’s head." Interestingly, the evidence for that statement that the authors discuss includes abnormal proteins in cerebrospinal fluid (the fluid that bathes the brain), antibodies directed against neurons (the main type of cell in the brain), and abnormal results from brain imaging studies. So even though the authors first say that chronic Lyme disease isn’t “all in one’s head” the studies they cite to show that the condition is a distinct illness all involve abnormalities in the nervous system and brain.
Similarly, an article in Elle was titled “Chronic Fatigue Syndrome Is Not All In Your Head," but the patient who was the subject of the story was successfully treated with an evidence-based psychological intervention—cognitive behavioral therapy.
In some cases, “you have depression” is heard as “it is all in your head,” meaning that one is making up or at very least exaggerating symptoms, perhaps to get out of having to work or go to school. Depression is of course a brain disorder, so it is true that the cause of depression is “in the head.” Still, mental health clinicians and their patients with depression have no doubt it is a very real condition. Fortunately, depression is also a treatable condition, thanks to a variety of evidence-based psychosocial and pharmacological interventions like cognitive behavioral therapy and antidepressant medication.
We do not know if contested illnesses like CFS, chronic Lyme disease, and fibromyalgia are in fact forms of psychiatric illness, but by railing against that possibility, people who have these conditions may be accepting a stigmatized view of mental illness as “unreal.” The brain is by far the most powerful organ in the body, exerting control over every other organ including heart, lungs, and the immune system. It is also a highly vulnerable organ, its incredible complexity making it prone to a vast array of abnormalities.
Research may someday demonstrate that chronic Lyme disease is primarily an infectious disease, fibromyalgia a muscle disorder, and chronic fatigue syndrome the result of immune system dysfunction. Or that research may show that, like depression, those conditions are fundamentally caused by malfunctions in the brain, a category of illness we call “psychiatric.” That would not make any of those illnesses any less real, painful, or, hopefully, amenable to evidence-based treatment.
It is time, then, to get over the fear that a psychiatric cause for an illness is somehow a dismissal of its “realness” or severity. Instead, we need to remember that psychiatric illnesses are themselves real and serious, even if they are mostly “all in the head.”
LinkedIn Image Credit: Rocketclips, Inc./Shutterstock




