Depression
Could Gut Microbiome Imbalance Play a Role in Depression?
New research shows links between imbalanced gut microbiota and depression.
Posted August 22, 2023 Reviewed by Davia Sills
Key points
- New research shows signs of energy metabolism disturbances in the guts of people with depression.
- Unhealthy eating patterns could increase a person's risk of depression.
- Making certain dietary changes and supplementing with probiotics could help balance the microbiome.

New research published in JAMA Psychiatry suggests a link between the disrupted gut microbiome and blood microbiome and depression. Researchers compared 6,811 individuals with lifetime major depression and 4,370 individuals with recurrent depression with people without depression and found that there were energy metabolism disturbances in the guts of people with depression. Researchers found that there were changes in the gut metabolites consistent with the presence of certain bacteria in the gut, including Clostridiales, Proteobacteria/Pseudomonadota, and Bacteroidetes/Bacteroidota.
A recent review in the Lancet also supports the increasing number of clinical studies that highlight disruptions in the gut microbiota, known as gut dysbiosis, associated with the onset and progression of depression. This effect is thought to be mediated by the gut-brain axis.
Many other studies show a link between unhealthy patterns of eating and depression. Eating fried food, processed meat, refined grain, high-fat dairy, and processed snacks has been linked to an increased risk of depression. Even though these studies do not definitively prove a cause-effect between diet and depression, they do suggest a new target for antidepressant treatment, including considering probiotics, prebiotics, and dietary changes.
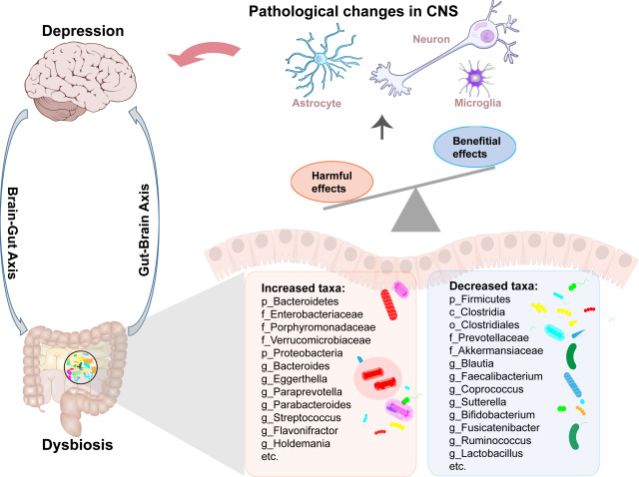
The link between an imbalanced gut and depression could be a vicious cycle—unhealthy eating patterns from depression can worsen a disrupted gut microbiome, which could then lead to persistent and worsened inflammation and depressive symptoms, even if diet had not been the initial underlying cause of the depression.
Another interesting finding is that antidepressant medications such as selective serotonin reuptake inhibitor antidepressants (SSRIs) and tricyclic antidepressants actually change the microbial diversity and composition in the gut, which could help explain some of their antidepressant effects.
What kind of dietary changes would support a healthy gut?
The Mediterranean diet highlights olive oil, whole grains, vegetables, beans, and omega-3 fatty-acid-rich fish and is filled with polyphenols and fibers. This diet has been associated with higher gut microbial diversity, lower levels of gut inflammation, and lower chances of a leaky gut.
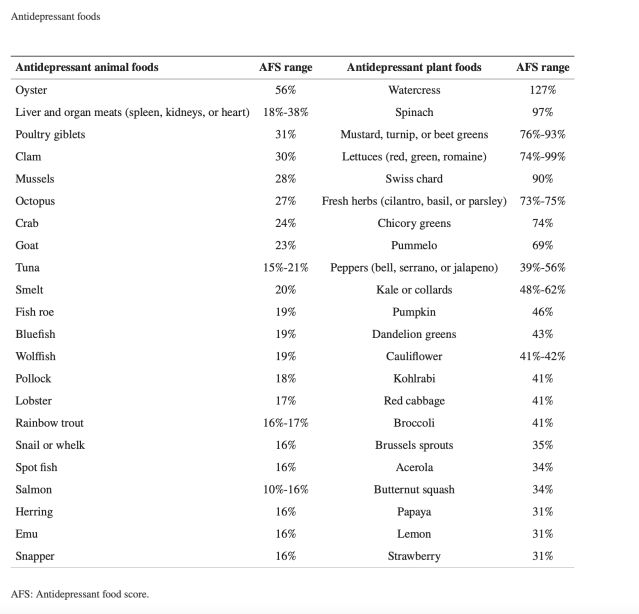
Researchers have also suggested a diet packed with 12 antidepressant nutrients: folate, iron, long-chain omega-3 fatty acids (EPA and DHA), magnesium, potassium, selenium, thiamine, vitamin A, vitamin B6, vitamin B12, vitamin C, and zinc. The highest-scoring animal foods were oysters, mussels, seafood, and organ meats. The highest-scoring plant foods were leafy greens, lettuce, peppers, and cruciferous vegetables.
In addition to making dietary changes, there are additional possibilities for balancing the gut microbiome, such as probiotics. Randomized control trials have demonstrated the benefit of certain probiotic species to help treat depression, including Lactobacillus helveticus, Lactobacillus rhamnosus, Bifidobacterium longum, and Bifidobacterium breve CCFM1025.
Ultimately, it is likely that the most effective dietary or nutritional supplement changes will need to be personalized and based on targeting the gut microbiome composition of the individual. The research continues to support the concept that gut microbiota plays an essential role in overall health, including mental health.
Copyright Marlynn Wei, M.D., PLLC © 2023
References
Amin N, Liu J, Bonnechere B, et al. Interplay of Metabolome and Gut Microbiome in Individuals With Major Depressive Disorder vs Control Individuals. JAMA Psychiatry. 2023;80(6):597–609.


