Autism
Autistic Brains Function Oppositely to Psychotic Ones
First direct brain imaging confirms the diametric model.
Posted March 20, 2018
According to the diametric model of mental illness, superficially similar social deficits in autism spectrum disorder (ASD) and psychotic spectrum disorders such as schizotypal personality disorder (SPD) have opposite causes: hyper-mentalizing in the latter case, and hypo-mentalizing in ASD. In other words, while autistics don’t mentalize enough, psychotics mentalize too much; where autistics don’t seem to have minds at all, psychotics suffer from cancers of the minds they do have.
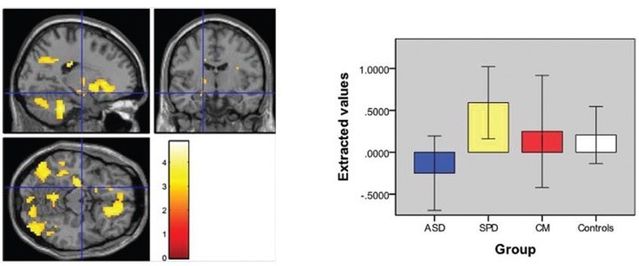
But is it true? In the first such study to directly do so, the researchers compared deficits in social cognition in 28 people with ASD and 21 with SPD, along with 33 controls. They tested whether such deficits are associated with different underlying brain activity using brain-imaging (fMRI). They employed a social judgment task (assessing approachability from faces) on which they had previously shown impaired performance in ASD and schizophrenia. The researchers hypothesized that individuals with ASD and those with SPD would show impaired social judgment compared to controls, but that, consistent with the diametric model, those with SPD would show increased activation of these brain regions while making social judgments whereas the opposite pattern would be seen in ASD (below).
The researchers report that
The clinical groups all showed similar patterns of impairment compared to controls in negative symptoms and the social cognition tests, but clear differences were seen between the ASD and SPD groups using fMRI during the social judgment task. Differences between the ASD and SPD groups were also seen in the relationship between amygdala activation and positive symptoms. Our findings demonstrate that apparently similar clinical and neuropsychological features may be associated with quite distinct underlying brain mechanisms.
—Just as the diametric model predicts. They add that
Although we did not identify clear group differences between either the ASD or SPD groups and the controls, results in the controls tended to lie between the 2 clinical groups, as did the findings for the CM [co-morbid] group [figure above]. Given this, and the above, we suggest that our findings are consistent with the hypo- and hyper-mentalizing theory of ASD and schizophrenia. Further evidence for distinct patterns of pathophysiology comes from our finding that increased activation in the left amygdala is associated with increased positive symptoms in SPD, whereas the reverse is true in ASD. These opposite patterns of correlation are consistent with the hypo- and hyper-mentalizing theory of the autism and schizophrenia spectrums with the SPD group developing psychotic symptoms due to over-activation of amygdala, whereas the ASD group develops such symptoms due to under-activation of this region.
They conclude that “our results are in keeping with the idea that the schizophrenia and autism spectrums represent diametrical disorders of brain development, at least in regard to social cognition.”
As to the clinical implications:
Irrespective of the exact nature of the underlying process, the differences we report carry important implications for clinical practice and classification. In particular it is important to note that clinical phenotypes can appear similar but arise from very different mechanisms and may therefore require quite different treatment approaches. This raises the prospect of developing treatments targeted at mentalizing styles, as opposed to clinical symptoms…These findings also highlight the importance of considering SPD as a differential diagnosis for ASD and vice versa; it is therefore important that diagnostic services where these conditions may be met, especially those working with adults, contain access to skilled professional assessment of both sets of disorders.
Finally, the study casts some light on the fraught issue of co-morbidity: cases which allegedly show signs and symptoms of both types of disorder:
We also identified people who met criteria for both ASD and SPD. This is consistent with previous work which reported that 23 percent of people with ASD met criteria for SPD. These “comorbid” individuals were more symptomatic than those with either condition alone, highlighting the importance of their identification. Interestingly, the fMRI findings for the CM group showed differences compared to the ASD group suggesting that they do not simply suffer from severe ASD. In contrast, there were no significant differences between the CM and SPD groups, which may indicate that they have a form of SPD.
I agree entirely. In psychiatry, thanks to brain-imaging like this also flagged up in previous posts, the Middle Ages are finally drawing to a close. Indeed, you could see the diametric model as the equivalent of the Copernican one, and brain-imaging that of the telescope astronomy which supplanted the horoscopes of the astrologers.


