
Stress
COVID Exhaustion
Understanding the stress response behind our fatigue—and what to do about it.
Posted June 30, 2020
The novelty of COVID-19 has definitely worn off.
When there is something new or unknown, even if it’s potentially scary, our brains light up in anticipation. Chemically, our bodies treat the expectancy of fear the same way as excitement. It’s why so many people love horror films. The anticipation of being scared is thrilling. But it’s nice at the end of the film to be able to snuggle into your safe bed, eat some popcorn and come back to a reality that isn’t filled with vampires, or zombies, or serial killers hiding in your closet.
But what happens when the fear lingers? When that killer invisible virus truly might be floating around and stalking you at every turn? Here is where we need to better understand how our bodies approach lingering stressors and how we can intervene in fear in order to remain productive, healthy, and hopeful.
Stage One – Adrenaline Rush
When we first learned about the coronavirus, we all likely experienced some hit of adrenaline.
This could be exciting!
I wonder how long I’ll be able to step away from work?
Sweet, I don’t have to get back on an airplane for at least the next month!
Despite already having some awareness of the dire consequences that might arise from its uncontrolled spread, COVID delivered something new to focus on that was separate from our regular day to day struggles. And because it was anticipatory fear, it was almost enjoyable (even if that sounds a bit sick to say now).
The physiological equivalent to this experience during a stress response is when we first experience a hit of adrenaline. Adrenaline is the initial neurotransmitter released in a challenging situation. It pulses through our body immediately sharpening our focus, reflexes, and responses. We take action without even knowing we are going to do so. This is the experience you might have had when you made that instinctive swerve to avoid a last-minute head-on collision. We feel almost superhuman in the moment — surprised by how powerful, focused, and confident our decisions were.
For the majority of Americans, I would describe this phase in our COVID experience as lasting through the end of March. From the time we initially became aware of this pandemic, through sometime in March, we were on our game. We made pivots. We quickly took action to get kids pulled from schools. We stayed on top of daily news from the Coronavirus Taskforce. And of course, if we could get our hands on it, we bought way too much toilet paper and hand sanitizer.
This phase came and went quickly, just like adrenaline does in the body.
Stage Two – Resistance
Cortisol, the main stress hormone for humans, comes surging in moments after adrenaline to help sustain the stress response. If you’ve ever jumped from a loud noise only to turn and realize it was just a car behind you backfiring, you’ll notice that the effects of adrenaline wear off nearly as quickly as they come on. So what happens if the threat is more sustained? That’s where cortisol takes over to champion the fight for survival.
Cortisol is a complex hormone that is involved in numerous daily metabolic functions. It plays important roles in memory, mood, and motivation. During a sustained stress response, cortisol works to divert resources away from non-essential functions (i.e. growth, reproduction, digestion) in favor of more immediate responses to quell the threat (i.e. increasing nutrients available to power muscles and repair damaged tissues, reducing pain perception). This cortisol powered “resistance system” to respond to a stressor is highly effective in the short-term but it is built to turn off or downregulate only when the threat has passed. Which leads to the logical question…
What if the threat isn’t a tiger, or a battle, or any other short-term challenge that our ancestors must have surely faced, but rather a sustained, ongoing, continually triggered challenge?
From early April through most of May, I think a lot of us found ourselves in this resistance phase of our stress responses. We realized that COVID-19 wasn’t a backfiring car and was going to present some longer-term challenges. We stopped reacting with panic-buying behaviors and began to put in a longer-term strategy. We would resist this virus and overcome together.
We bought Zoom licenses and masks. We altered our eating habits and worked different shifts with alternate teams, and sometimes with our children crawling on us in the middle of a conference call. We shut down non-essential functions in our life and did our best to pour into the things we needed to do to survive (for a while). But that “while” has lasted a bit longer than most of us anticipated.
Stage 3 - Exhaustion
The threats for which our stress response system was designed were short-lived. When a stressor persists in the manner that COVID has, our bodies are continuously flooded with cortisol. All the things that cortisol does that are adaptive in the short-term begin to wreak havoc on systems during periods of longer exposure.
For example, cortisol makes sugar more readily available in our bloodstream so that our muscles can use it to escape the threat. But we can’t outrun or outfight COVID. Cortisol simultaneously increases our desire to seek out sweet foods to replenish the sugars we (supposedly) burned escaping or fighting off the threat. So, it might be less of a surprise to know that weight gain and diabetic complications both coincide with long-term stress.
Cortisol also helps regulate sleep cycles. With overexposure to cortisol, we sleep less which exacerbates our stress, anxiety, and depressive moods.
Essentially all the things we need to be doing to fight against reaching this stage of exhaustion, our hormones are telling us not to do. If you’re languishing in this exhausting phase that most of us reached somewhere in early summer 2020, there is hope.
Stage 4 – Adaptation & Recovery
I personally would like to insert this stage before any of us ever reach the stage of exhaustion, but if you missed the opportunity to prevent jumping into the exhaustion phase, you can still protect yourself from worsened spiraling and adapt moving forward. Here is where we have the opportunity as humans to think beyond our biology. Essentially everything your hormones are telling you to do is the opposite of what you need to be doing to adapt and recover during this COVID induced cortisol crisis.
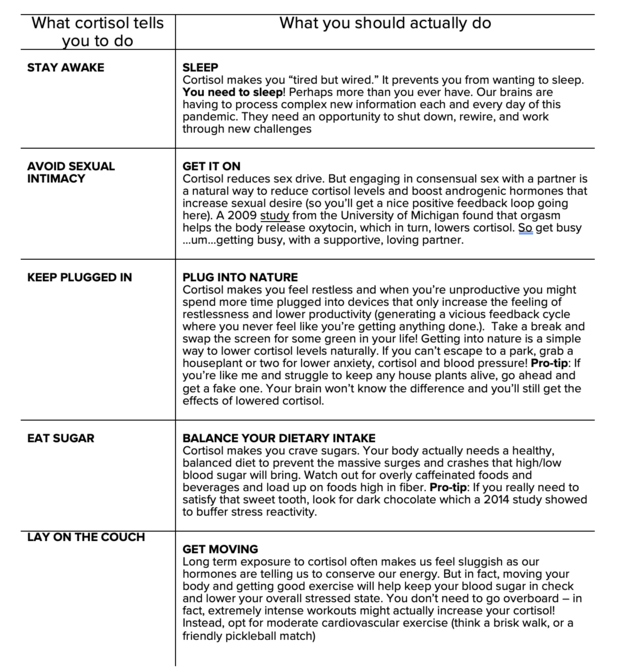
We don’t have to feel trapped in this state of COVID/cortisol exhaustion. While it’s natural for most of us to have ended up here, we aren’t prisoners to our biology. We all have the power to move beyond our stress-induced physiological reactions and override our outdated instincts. Here’s to breaking free of your biology toward something better!



