Health
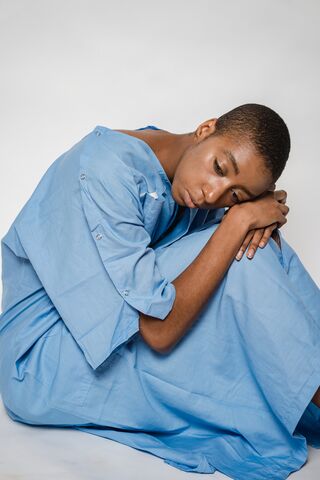
Medically Ill and Emotionally Struggling
A problem that is all too common, and is commonly ignored.
Posted October 29, 2021 Reviewed by Tyler Woods
Key points
- Emotional suffering and mental illness are common consequences of medical illness.
- The mental components of medical illness are usually not attended to.
- Many studies have shown that mental health treatment helps alleviate the emotional fallout of illness.
- Mental health professionals should be members of treatment teams to monitor patients and deliver needed care.
I opened my psychiatric office in 1989, right across the street from our local hospital. I joined the hospital staff, did consultations on in-patients, and joined the local medical society.
My plan was to make my presence as a psychiatrist known to the medical community. This, I hoped, would coincide with the blossoming knowledge about psychiatric problems among medical patients. Physicians were just beginning to learn that cancer, cardiac, and rheumatology (arthritis) patients, among others, commonly had depression, anxiety, and other mental health issues. This may seem obvious now, but it was not always so.
Although I did receive many patient referrals, the flood of people with these medical conditions never materialized. Not even in the following 23 years of my practice. Little did I know that I would join not one, but two classes of these patients: rheumatology and cancer. In the unplanned way that many journeys unfold, I would learn about this issue from both sides.
I am disappointed to report—from both sides of the issue—that medical patients frequently develop mental health problems (especially those with certain diagnoses) and that they are largely left unattended. What was blossoming when I began my practice is now a highly developed area of study. Research shows that cardiac patients are at a higher risk of death when they are also depressed; that rheumatology patients struggle with how to function and how to cope with pain and disability; and that cancer patients deal with multiple medical complications and the obvious fear of death.
There are many things we could add to this list, such as disfigurement, being kept alive by a piece of technology (e.g. an internal cardiac defibrillator), or isolation and poor quality of life.
The strength of these many studies, along with my experience in hospitals and rehab facilities, left me convinced that a mental health professional should be part of any team that manages the care of cardiac, rheumatology, cancer, and other patients who are likely to suffer mental health complications of their illness. Unfortunately, this is rarely the case.
A Personal Experience of Severe Illness
My personal experience began with a rheumatological disorder that became very active in my mid-forties, and by my fifties left me unable to work. My career in treating psychiatric patients was over. I dealt with multiple surgeries and medical complications that were quite difficult, over and above the illness itself. I thought my final joint surgery (a second hip replacement) would stabilize my situation. But this was plagued with complications, some life-threatening, and was topped off by a CT scan that found advanced cancer.
My cancer treatment was like that of many others, a demanding ordeal. Throughout the almost two years that have passed, my wife and I naturally feared for my life. At this time, it seems like I have beaten the odds.
I bring up the details of my illnesses only to make the following point: although my care teams were usually quite good, I can honestly say that at no point did anyone ask me how I was doing emotionally. There were even times when I cried, and this still did not elicit questions about my state of mind. Something is clearly wrong when patients who have suffered great losses, significant pain, or may not have long to live, are left to deal with their fear and anguish by themselves. I do not think the problem is that the medical staff do not care. Rather, they have no time to sit and talk, and even if they did, they have no training in how to help.
We Know That Treatment Works
Mental health professionals have the expertise. Psychiatric interventions cannot reverse diagnoses, difficult treatments, or losses. What they can do is help patients cope. This can take the form of helping with anxiety, depression, grief over losses, coping with changes and, building meaning back into life. As with the diagnoses mentioned above, these interventions have been studied, and indeed work. In fact, treatment of depression and anxiety can even help lessen pain. (We should leave the care of terminal patients to hospice, as their team approach has proven best for this group's needs).
Why then, aren’t these treatments routine? There are some clear candidate answers. One is that specialists are not trained enough in the mental health aspects of their specialty. Another is time pressure. Physicians and other staff are under tremendous strain to perform and document many clinical activities. This leaves important conversations left undone. Last is the lack of availability of mental health professionals to refer to. More and more clinicians are dropping insurance as billing requirements become burdensome or they are simply fully booked.
Emotional Pain, Obvious but Still Ignored
These problems are all quite real. But I am left unsatisfied that we have explained such a glaring chasm in meeting the psychological needs of our sickest patients. I believe we are left, not with the stigma of mental illness, but the lack of awareness that it exists, is common, and occurs predictably during stressful periods in our lives.
For many, mental illness remains something that happens under the cover of secrecy, to other people. It lives in the shadows, is always “crazy,” and no doubt is partly their own fault. This is a cynical assessment, but it is an honest one, made from years of discussions overheard and pointed directly at me because I am a psychiatrist.
I have no easy solution to the society-wide problem other than education. But for the medically ill, who commonly suffer mental health problems as a consequence of their illnesses, there must be an experienced, well-trained mental health professional embedded in the teams that take care of them. Pastoral counselors, who are in most hospitals, perform an important service, but it is not this. Staff should not wait until someone voices suicidal thinking or becomes agitated to ask for a psychiatric consultation. We now know enough to predict when someone is likely to be struggling, and it only takes a sit-down conversation to tell you what you need to know.
This is just one part within the large area of under-recognized and under-treated mental health problems. Nothing short of continually voicing the reality and commonality of mental illness will get it the attention it deserves.




