
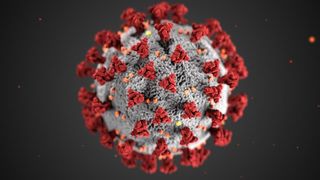
Coronavirus Disease 2019
Why Do Symptoms Vary So Much?
Viruses go everywhere. So do the symptoms they cause.
Posted April 5, 2020 Reviewed by Jessica Schrader
Viruses go everywhere. Viral symptoms can happen in any organ and produce elements like fever that are system-wide. Fortunately, your immune system works often brilliantly in every part of your body. That’s why in Vo, the only town in the West where everyone was tested for COVID-19, 3% were found to be infected at the beginning of the epidemic, and 70% were either completely asymptomatic or had very “mild” symptoms.
What constitutes mild? Feelings of malaise, tiredness, weakness. Just not feeling right. Maybe a headache. Loads of people did not experience anything. In the Dutch studies in Breda and Tilburg, which looked only at hospital workers who were symptomatic for a recent upper respiratory infection, half of those who tested positive had no fever. Two-thirds kept working. Based on Italian data, medical statistician Carlo Lo Vecchia thinks 5-10 million Italians may already have been infected. Most will have had very little clue. We’ll see if oncoming antibody studies prove him right.
But viruses have their own characteristic pattern of infection. Understanding that allows one to understand why Sars Cov 2, our present-day nemesis, can provoke anything from no symptoms to sudden collapse and death.
Sars Cov 2 has many similarities to the original SARS, which proved so lethal nearly 20 years ago before it rapidly disappeared. The virus latches onto special receptors on cell membranes at the back of your throat. Perhaps 100 to 500 viral particles working in concert are enough to infect and invade. Viral proteins merge with cellular membranes in your cells as they take over and produce innumerable viral copies. As more cells get infected, the cellular debris drops down through your throat into your lung. It’s in the lower lungs that Sars Cov 2 coronavirus is doing its most lethal work.
A large part of how you feel and how sick you get is linked to your immune response. You can think of the virus as an “invading army,” where a larger cohort will wreak more damage. That is true for flu and other viruses, and may explain why some point outbreaks are so much faster and more lethal than others; ten million viral particles coming at you at once is a lot harder to fight off than five hundred.
But it’s also a matter of how you fight. The immune system is immensely complex, with cascades of different effective measures. Most of the symptoms we get, like scratchy throat and fever, occur because of immune response.
Very importantly in COVID-19, immune response in certain individuals goes into overdrive. What’s called a “cytokine storm” may be one of the major reasons some patients go from looking relatively healthy to going into shock in a matter of hours.
The results, like with the original SARS, are far worse with older folks than younger ones. As with most infections, some people will fight off heavy viral loads with no symptoms, while others who see relatively few viral particles will rapidly become ill. Our individual immune responses vary enormously, including from pathogen to pathogen; you might fight off coronavirus very well, but not flu; bacteria like pneuomoccus, but not haemophilus. The variation is great, including how easily a virus gets into our blood.
Once viruses get a real toehold, they usually spread through the blood. (Some can’t. Rhinovirus, which causes a lot of colds, doesn’t like temperatures above 33 degrees centigrade.) In most circumstances, the numbers of viral particles found in blood are very small. Chances are extremely high you won’t get COVID-19 through a blood transfusion.
But most viruses causing upper respiratory infections often get a few particles into the bloodstream. If people have a bad cold and you do a spinal tap, often there will be a few white cells present. Officially you have “meningitis.” What you’ll know is that you had a bad cold.
Yet with more severe infections, viruses travel through blood and lymph almost everywhere—to the heart, brain, spleen, liver. That may explain why quite a few people with COVID-19 will have nausea and diarrhea, while others develop severe disease in their kidneys. Please remember that our immune system is literally everywhere (the brain component works a bit differently from the rest), so we can have system-wide symptoms, like fever, from infections that may be very localized.
In the end, the level of viral load in the blood may tell clinicians who will have the most severe, lethal infections. It’s a big factor in treating AIDS. It also appears to matter in SARS infections.
Testing in a clinically useful manner for coronavirus blood levels is quite a ways off.
Bottom Line
Viral infections start in one place, but often get into the blood, where they travel everywhere. Most of the severe infectious risk of COVID-19 is in the lungs, but not all. How your individual immune system responds is critical.
And most of the time, it works extremely well. If present data hold, many or perhaps the majority of folks infected never knew. We won’t know the truth until we do what places like South Korea and Italy’s Veneto region have done effectively: test and track. We can’t do that soon enough.



