Eating Disorders
Psychological Maintenance Processes of Binge-Eating Disorder
A new cognitive behavioral theory of binge-eating disorder.
Posted September 9, 2024 Reviewed by Michelle Quirk
Key points
- Cognitive behavioral theory integrates psychological processes that maintain binge eating and higher weight.
- Binge-eating disorder includes overvaluation of shape, dysfunctional dieting, and mood changes.
- BED also includes dysregulated eating, internalized weight stigma, and unrealistic weight goals.
Binge-eating disorder (BED) is characterized by recurrent binge-eating episodes not followed by the regular use of compensatory behaviors. Research indicates a lifetime prevalence of 0.42 percent in men and 1.25 percent in women, with an overall rate of 0.85 percent. Although BED can affect individuals of normal weight, it is more commonly found in those with higher weight.
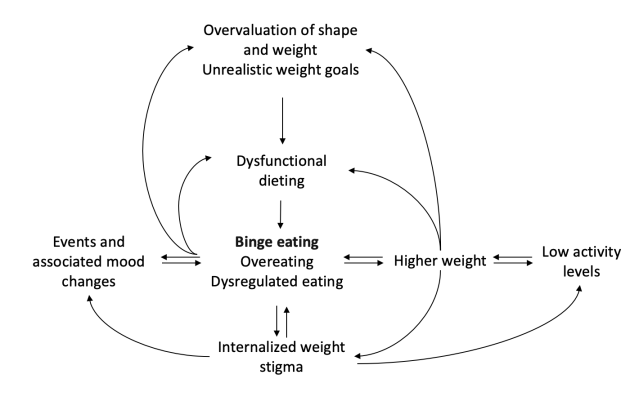
In this post, I present a new cognitive-behavioral theory of BED, which integrates well-established cognitive-behavioral mechanisms that sustain binge-eating episodes with additional cognitive and behavioral factors that contribute to the maintenance of higher weight (Figure 1). While not all these maintenance factors are present in every case of BED, each case involves a combination of these elements.
Events and Associated Mood Changes
Life events and associated mood changes frequently trigger and sustain binge-eating episodes in individuals with BED. This link between life events, emotional changes, and binge-eating can be understood through several key observations:
- Food may be used as a distraction from adverse events and problems.
- Food can help alleviate negative emotional states.
- Food often serves as a means of self-gratification.
However, despite the initial relief from negative emotions, binge-eating episodes often result in feelings of guilt, anxiety, and depression. These negative feelings can then trigger subsequent binge-eating episodes, creating a vicious cycle.
Overvaluation of Shape and Weight
A person is described as having an overvaluation of shape and weight when they predominantly, and sometimes exclusively, judge their self-worth based on their body shape, weight, and their ability to control them. This characteristic is present in approximately 50 percent of individuals with BED.
In BED, overvaluation of shape and weight is often accompanied by intermittent dysfunctional dieting aimed at weight loss, which, in turn, increases the likelihood of binge-eating episodes.
Unrealistic Weight Goals and Primary Goals
Currently, no treatments, except for bariatric surgery, achieve an average long-term weight loss of more than 15 to 20 percent of initial body weight. However, many individuals seeking weight loss have unrealistic expectations about how much weight they can lose. Studies conducted in Italy indicate that many people starting weight-loss treatment aim for an average weight loss of 32 percent.
Additionally, these individuals often have other "primary" goals they hope to achieve through weight loss, such as improving interpersonal relationships, boosting self-confidence, or finding a partner or a new job.
There appears to be a link between these unrealistic weight and primary goals and treatment discontinuation. Unrealistic weight goals can lead people with BED to alternate between binge eating and extreme weight-control behaviors, each behavior fueling the other through the mechanisms described below.
Dysfunctional Dieting
Some individuals with BED attempt to control their weight and alter their body shape by intermittently adopting dysfunctional diets characterized by extreme, rigid dietary rules. This pattern of dieting makes further binge-eating episodes almost inevitable. The stricter and more numerous the dietary rules, the more likely they are to be broken. When this happens, individuals often interpret their inability to adhere to these rules as evidence of their lack of self-control rather than recognizing that their dietary rules are too strict or extreme.
This "all-or-nothing thinking" leads to the temporary abandonment of efforts to curb calorie intake, resulting in another binge-eating episode. This cycle of rigid dieting, inevitable rule-breaking, self-blame, and subsequent binge eating perpetuates the disorder and makes sustainable weight control even more challenging.
Overeating and Dysregulated Eating
Between binge-eating episodes, individuals with BED often overeat, and their eating habits tend to be dysregulated, lacking flexible moderation in food intake. Dysregulated eating behaviors may include the following:
- Skipping meals
- Frequently snacking or grazing between meals
- Consuming oversized portions and “junk” foods high in calories, saturated fat, sugar, and/or salt (e.g., hamburgers, hot dogs, fried chicken, French fries, sugary drinks, processed desserts, pizza)
This pattern of overconsumption and dysregulated eating often results in an excessive daily caloric intake, contributing to the onset and maintenance of higher weight.
Higher Weight
Genetic predisposition to higher weight, combined with binge eating, overeating, and dysregulated eating, explains why higher weight is common in individuals with BED. As illustrated in Figure 1, higher weight increases the risk of developing internalized weight stigma. This stigma fuels the overvaluation of shape and weight, unrealistic weight goals, and the intermittent adoption of dysfunctional dieting practices. The cycle perpetuates dysregulated eating, overeating, and binge-eating episodes. Consequently, higher weight not only predisposes individuals to BED but also exacerbates the disorder through these interconnected mechanisms.
Sedentary Lifestyle
A significant subgroup of individuals with BED and higher weight engage in minimal physical activity throughout their day. This low energy expenditure contributes to the development and maintenance of higher weight. The resulting higher weight makes physical activity more difficult and less enjoyable, perpetuating a cycle of inactivity and weight gain.
Internalized Weight Stigma
Internalized weight stigma occurs when individuals adopt society’s negative weight stereotypes as their own, leading to negative self-beliefs. These individuals perceive themselves as inferior to those who can control their weight, resulting in self-critical thoughts such as "I'm so lazy," "I have no willpower," "I hate myself for not having any self-control," "I'm a failure," and "I am ugly and disgusting."
People with internalized weight stigma often manage their negative emotions through binge-eating episodes and overeating. They derive little pleasure from physical activity and sports, tending to avoid them. Their low self-efficacy—the belief in their capacity to perform behaviors necessary to achieve specific goals—further hampers their attempts to control eating and weight. This lack of confidence can lead to avoidance of treatment due to fear of failure.
Conclusions
The new cognitive behavioral theory of the maintenance of BED is innovative in that it acknowledges the need to address dysregulated eating and overeating between binge-eating episodes, as well as a sedentary lifestyle, unrealistic weight-loss goals, associated primary goals, and internalized weight stigma. According to this model, the treatment of BED should enable patients to address and overcome the primary mechanisms underlying their disorder in a personalized and flexible manner.
References
Cooper Z, Calugi S, Dalle Grave R. Controlling binge eating and weight: a treatment for binge eating disorder worth researching? Eat Weight Disord. 2019;25(4):1105–1109. doi: 10.1007/s40519-019-00734-4.
Dalle Grave R, Calugi S, Sartirana M. Cognitive behaviour therapy for binge-eating disorder. Springer Nature. In press.




