Hormones
Stabilize Your Mood with Food
How to get off that invisible hormonal roller coaster
Posted June 28, 2017 Reviewed by Ekua Hagan

By now you’ve probably heard that sugar is bad. It rots our teeth, makes us fat, and leads to devastating diseases like diabetes and heart disease. But how does sugar affect our mental health?
There are at least three key ways that high-sugar diets can contribute to mood, concentration, and energy problems: hormonal destabilization, inflammation/ oxidation, and insulin resistance.
In this post, we’ll concentrate on the hormonal pathway—how sugar can cause mood swings and other emotional issues by wreaking havoc with our natural hormonal balance.
So first, a definition of sugar—because it’s frequently misunderstood.
How Much Sugar Do You Actually Eat?
Most people, even those who have made the good decision to stop eating sugar, are still eating substantial amounts of sugar throughout the day without realizing it.
All sweet and starchy foods, whether they are whole foods or refined junk foods, turn into the same two simple sugar molecules in our bodies: glucose and fructose. And it just so happens that our liver turns fructose instantly into glucose, so, all roads lead to glucose —the sugar that cruises through our bloodstream. Dozens of foods are sugar in disguise, including some that aren’t sweet at all: flour, cereal, fruit juice, beets, potatoes, and even dried fruit are quite high in natural sugars, even though they have “no sugar added.”
Glucose molecules from a sweet potato and glucose molecules from cotton candy are identical—so why should we worry about which kinds of carbohydrates we eat?
The reason why “refined” carbohydrates such as sugar and flour are less healthy than whole carbohydrate sources like peaches and carrots is that refined sources typically contain more glucose per serving AND tend to break down into glucose faster. When we eat too many concentrated sources of rapidly-digestible carbohydrates, blood glucose spikes sharply, triggering an equally strong spike in insulin to bring blood glucose back down.
Sugar vs. Starch
Take a look at this experiment showing how blood glucose and insulin behave when sugar (sucrose) is eaten with every meal (left) and when starchy foods like white rice, white bread and potatoes are eaten with meals (right):
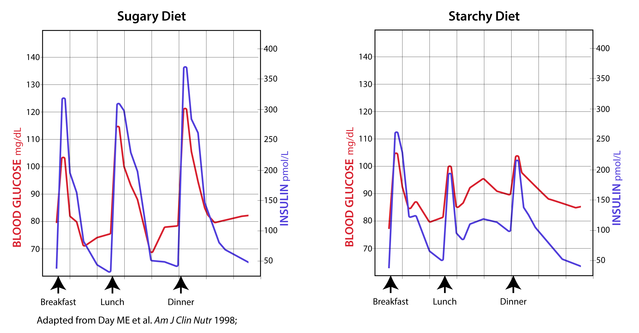
Even though the effects of the sugary diet are more dramatic, you can see that carbohydrates don’t have to be sweet to cause peaks and valleys in blood sugar.
So, you may wonder—since insulin normalizes blood sugar so quickly, why worry?
Insulin's Secret Powers
Here’s the problem: insulin is not simply a blood glucose regulator, though even many doctors continue to think of it that way. Insulin is actually a master growth hormone; when it peaks, it puts the body into growth and storage mode. One of the ways it does this is to turn fat-burning enzymes OFF and fat-storage enzymes ON, which is why high-sugar diets can be so fattening.
In its role as master growth regulator, insulin orchestrates the activity of numerous other hormones, including the blood pressure regulating hormone aldosterone, reproductive hormones like estrogen and testosterone, and stress hormones like cortisol and adrenaline. So, every time your insulin goes up and down, all of these other hormones go up and down in response, with potentially profound effects on your mood, metabolism, appetite, blood pressure, energy, concentration, and hormonal balance.
Let’s zero in on one of these glucose-insulin spikes:
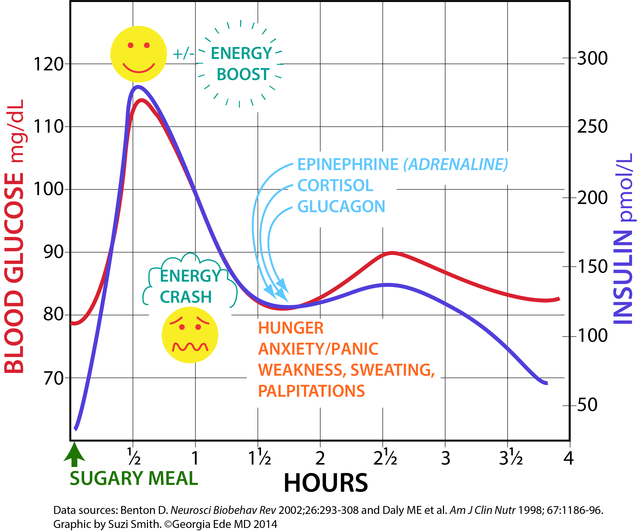
Let's say you start off your morning with a food rich in "fast" carbohydrates (like orange juice, a bagel, or home fries):
- Within a half hour, your blood sugar spikes, which may give you an energy boost.
- Your pancreas immediately releases insulin into your bloodstream to pull the extra sugar (glucose) out of your blood and squirrel it away into your cells.
- About 90 minutes later, as your blood glucose drops, you may experience a “sugar crash” and feel tired, unfocused, and hungry.
- In response to plummeting glucose, your body produces stress hormones that increase blood glucose and keep it from bottoming out.
Hangry Hypoglycemia
This multi-hormone reaction can cause some to experience physical and emotional distress between meals, often mistakenly characterized as “hypoglycemia” (low blood sugar). In fact, true reactive hypoglycemia is rare (except in those who take blood-sugar lowering medications). It’s not that blood sugar is dropping below normal between meals; it is that it falls rapidly or from a high peak, triggering an exaggerated stress hormone reaction.The stress hormones involved include glucagon, cortisol, and adrenaline—our “fight-or-flight” hormone.
How much adrenaline are we talking about? In the experiment below, researchers gave healthy teenage boys a glucose-sweetened beverage (containing about the same amount of sugar as you’d find in two 12-oz cans of soda):
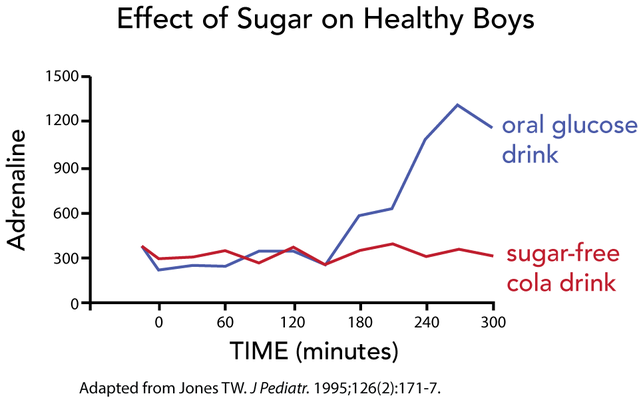
Four to five hours after the boys drank the sweetened beverage, their adrenaline levels QUADRUPLED, and they reported symptoms such as anxiety, shakiness, and difficulty concentrating.
The Invisible Hormonal Roller Coaster
Keep in mind that most of us eat refined carbohydrates at every meal, and usually between meals as well, translating into 3 to 6 major insulin spikes PER DAY. Eating this way puts us on an invisible internal hormonal roller coaster all day long (and even after we fall asleep). Age, metabolism, gender, genetics, diet, and activity level all influence what our internal roller coaster looks like and how we respond to it, but most of us eventually pay an emotional or physical price for eating too many of the wrong carbohydrates too often. Fatigue, difficulty concentrating, mood swings, binge eating, weight gain, irritability, anxiety, panic attacks, hormonal irregularities and insomnia are all possibilities, depending on the individual.
So what’s the solution? Eating six times a day? Meditation? Ativan? Ritalin? Lithium? Zyprexa?
How about starting by simply avoiding refined carbohydrates and sticking to a whole foods diet that minimizes big swings in blood glucose and insulin in the first place?
Unfortunately, that’s easier said than done. Sugar in all of its devilish disguises is delicious, cheap, everywhere, and more addictive than cocaine.
Behold the Power of Diet
It takes commitment and practice, but it is worth it. Look at the immediate difference a single meal made in the blood sugar, insulin and adrenaline levels of these overweight teenage boys:
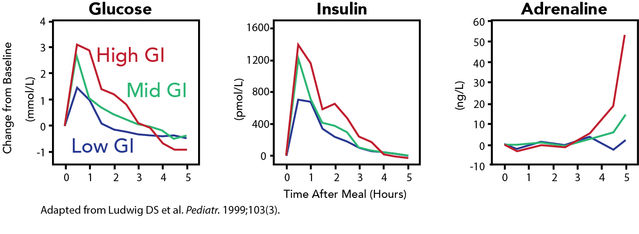
Dr. David Ludwig's research team was interested in understanding how the glycemic index (GI) of foods--a measure of quickly foods break down into glucose--affects metabolism. The team designed three breakfasts:
High-GI breakfast: instant oatmeal with sugar (sucrose) and 2% milk
Mid-GI breakfast: steel-cut oatmeal with fructose (a glucose-free sweetener) and 2% milk
Low-GI breakfast: vegetable-cheese omelet and fresh fruit
Notice that while sugar-free steel-cut oatmeal performed better than sugary instant oatmeal, it was the higher-fat, lower-carb, grain-free, sugar-free, whole-foods breakfast that was best at lowering glucose, insulin and adrenaline levels.
Grab the Wheel
Most of us don’t realize how much better we can feel—physically and emotionally—if we eat right. If you’re like most people, you’ve been misled about what a healthy diet truly is, so you’ve been consuming high-carbohydrate, fat-free foods like cereal, fruit juice and pasta every day that are actually working against your metabolism, your hormones, and your mood. You may think of yourself as a depressed or negative person, a high-strung stressball, or a fragile, moody sort who is easily overwhelmed—but maybe you're actually perfectly fine—or at least a lot better—underneath all that sugar.
I have certainly seen cases in my own clinical practice of people who stabilized their own mood without medication by removing refined carbohydrate from the diet or switching to a low-carbohydrate diet. Earlier this year I summarized this groundbreaking 2017 study for Psychology Today demonstrating that people with depression who made healthy changes to their diet--including removing most refined carbohydrate--saw an improvement in their mood.
What could it do for you?
Here’s a challenge: eliminate all refined carbohydrate for two weeks—just to see how you feel. There is a free list of refined carbohydrates on my website if you need it, and an infographic on my Psychology Today post about sugar and Alzheimer’s Disease to help you identify sources of hidden sugar in everyday foods.
To your good mental health!




