The Diagnostic and Statistical Manual of Mental Disorders (DSM) is a guidebook widely used by mental health professionals—especially those in the United States—in the diagnosis of many mental health conditions. The DSM is published by the American Psychiatric Association and has been revised multiple times since it was first introduced in 1952. The most recent edition is the fifth, or the DSM-5. It was published in 2013.
The DSM coexists with various alternative diagnostic tools, although these other guides are generally less commonly used in the U.S. The most widely consulted counterpart of the DSM, the World Health Organization’s International Classification of Diseases (ICD), covers mental health disorders along with a vast number of other health conditions. The ICD is the primary diagnostic tool for mental health professionals outside the U.S.

The DSM features descriptions of mental health conditions ranging from anxiety and mood disorders to substance-related and personality disorders, dividing them into categories such as major depressive disorder, generalized anxiety disorder, and narcissistic personality disorder. These disorders are grouped into chapters based on shared features, e.g., Feeding and Eating Disorders; Depressive Disorders; Schizophrenia Spectrum and Other Psychotic Disorders.
For each disorder category, the manual includes a set of diagnostic criteria—lists of symptoms and guidelines that psychiatrists, psychotherapists, and other health professionals use to determine whether a patient or client meets the criteria for one or more diagnostic categories. For diagnosis of major depressive disorder, for example, the current DSM states that a person shows at least five of a list of nine symptoms (including depressed mood, diminished pleasure, and others) within the same two-week period. It also requires that the symptoms cause “clinically significant distress or impairment in social, occupational, or other important areas of functioning,” along with other stipulations.
Updates to these diagnostic categories and criteria are made through a years-long research and revision process that involves groups of experts focusing on distinct areas of the manual.
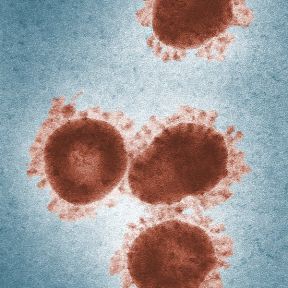
The DSM is important for several reasons. First, it creates a common language to describe mental disorders; developing consistency is key because diagnoses are primarily based on symptoms and family history rather than more objective measures like blood tests or brain scans.
Second, diagnosis makes it possible to study treatments for mental illnesses. When people present to mental health services, professionals need to have some guide as to which treatments will best address particular collections of symptoms. Third, diagnosis facilitates research into the causes of mental disorders. If research in Peru links depression with poverty, a common concept of depression is necessary to investigate similar links in Canada.
Diagnostic criteria help students and early-career professionals build templates of mental disorders that go beyond a layperson’s impressions—for instance that bipolar disorder describes abnormal moods sustained over weeks or months, not moods that shift over an hour or a day. The DSM establishes a common language for professional communication and research, not to mention insurance codes.
However, there are also ways in which mental health professionals don’t view the DSM as clinically useful. After seeing many patients, clinicians gradually form their own mental models of common diagnoses that might differ from the DSM, for example that the published criteria for a particular diagnosis is a little too wide or too narrow. In the end, clinicians may privilege the nosology of their own experience over the official manual that approximates it.
The criterion-based diagnoses listed in the DSM have improved consistency and reliability in classifying mental health conditions over time; clinicians around the world can now largely agree whether a particular patient “meets DSM criteria.” This shift in the DSM has been useful for research, in which the homogeneity of study groups is crucial.
Some believe that the failure to develop effective treatments for mental health disorders can in part be traced to a failure of classification, embodied by the long-standing reliance on the DSM. The DSM labels clusters of co-occurring symptoms and sorts them into disorder categories, but there is little evidence that these categories correspond to distinct biological realities. DSM categories may thereby hamper rather than facilitate psychology’s understanding of mental disorders.

The DSM has always been a lightning rod for debate about psychiatric diagnosis and classification. Since the 1950s, various categories of disorders have been added to the manual, altered, or removed altogether based on evolving clinical expertise and research and changes in the field of psychiatry, including a pivot away from psychoanalysis.
As the DSM is the dominant text for making mental health diagnoses in America, many of these changes are considered historically significant, such as when the DSM ceased to classify homosexuality as a form of mental illness in 1973. Other shifts have been controversial, including the omission of Asperger’s disorder from the DSM-5 in favor of a broader autism spectrum disorder category.
The DSM-5 organizes mental disorders into the following chapters: Neurodevelopmental Disorders, Schizophrenia Spectrum and Other Psychotic Disorders, Bipolar and Related Disorders, Depressive Disorders, Anxiety Disorders, Obsessive-Compulsive and Related Disorders, Trauma- and Stressor-Related Disorders, Dissociative Disorders, Somatic Symptom and Related Disorders, Feeding and Eating Disorders, Elimination Disorders, Sleep-Wake Disorders, Sexual Dysfunctions, Gender Dysphoria, Disruptive, Impulse-Control, and Conduct Disorders, Substance-Related and Addictive Disorders, Neurocognitive Disorders, Personality Disorders, Paraphilic Disorders, Other Mental Disorders, Medication-Induced Movement Disorders and Other Adverse Effects of Medication, and Other Conditions That May Be a Focus of Clinical Attention.
The DSM-5 departed from the previous version in several ways. A few of the key changes include:
• Eliminating the multi-axial diagnostic system that required clinicians to rate each client according to criteria other than their main psychological disorder.
• Replacing the diagnoses “Autistic Disorder” and “Asperger’s Disorder” with the overarching label “Autism Spectrum Disorder.”
• Establishing “Obsessive-Compulsive Disorders” as its own group of disorders rather than an anxiety disorder.
• Establishing PTSD as a “Trauma and Stressor-Related Disorder” rather than an anxiety disorder.
• Replacing the diagnoses "Alcohol Abuse" and "Alcohol Dependence" with the overarching label "Alcohol Use Disorder," characterized as mild, moderate, or severe based on the number of symptoms present. The same goes for other diagnoses related to addiction.
• Changing diagnoses with stigmatizing terminology, such as replacing the diagnosis “Mental Retardation” with “Intellectual Disability.”
• Removing the exception of bereavement for the diagnosis of Major Depressive Disorder.
• Adding the diagnosis “Mild Neurocognitive Impairment” to categorize cognition problems in old age.
• Reclassifying childhood disorders such as ADHD as neurodevelopmental disorders.
• Adding the diagnosis of “Binge-Eating Disorder.”
Some psychiatrists believe that elements of the DSM-5 are deeply flawed. “Excessive ambition combined with disorganized execution led inevitably to many ill-conceived and risky proposals,” writes Allen Frances, chair of the DSM-IV Task Force and a professor emeritus at Duke, which could lead to misdiagnosis and overprescribing, especially for children.
The most concerning changes of the DSM-5, Frances believed, include incorporating grief into major depressive disorder, diagnosing typical forgetting in old age as Minor Neurocognitive Disorder, and introducing the concept of behavioral addictions.
The International Classification of Diseases (ICD), published by the World Health Organization, is the best known and most popular alternative to the DSM. It contains diagnostic codes used for tracking incidence and prevalence rates, as well as for health insurance reimbursement, for mental and physical disease diagnoses.
Other alternatives to the DSM include the Psychodynamic Diagnostic Manual (PDM), Hierarchical Taxonomy of Psychopathology (HiTOP), Research Domain Criteria (RDoC), and Power Threat Meaning Framework (PTMF).
The Hierarchical Taxonomy of Psychopathology (HiTOP)—accounts for mental illness at multiple conceptual levels. It covers specific symptoms (such as avoidance, social anxiety, and suicidality) and traits (callousness, distractibility), but also more general factors with names such as Distress and Fear. The DSM, by contrast, tends to be categorical and binary.
The HiTOP model is dimensional: A person can score low, high, or somewhere in between on various measures. These severity scores can apply to the more general factors of psychopathology as well as to the narrower ones. As proponents of the model note, evidence suggests that most kinds of psychopathology lie on a continuum with normality.