Appetite
The Brain's Role in Losing Weight and Keeping It Off
The role of your brain in the process.
Posted March 30, 2023 Reviewed by Jessica Schrader
Key points
- Losing weight is difficult enough. Keeping it off can be even more problematic.
- Our brains are monitoring weight loss more than weight gain.
- Synaptic plasticity may account for the difficulty in keeping the weight off.
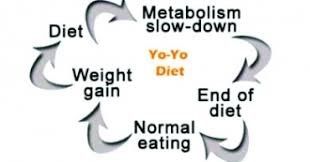
The CDC reports that between 2013 and 2016, almost 50% of adults in the United States tried to lose weight within a given year. The CDC also reports most of the people who are successful in losing unwanted pounds will put that weight back on, which often results in another attempt to lose weight. That repeated weight loss/weight gain/weight loss cycle is what is known as yo-yo dieting. Almost everyone knows, usually through painful experience, that getting the weight off is one thing, while keeping it off is a different thing entirely.
It is a common belief among nutrition experts and researchers who study our eating habits that almost everyone who loses weight will eventually gain it back. A report in Scientific American (Engber, 2020) states that almost all (his figure is 80%) of people who were successful in losing a significant proportion of body fat will be unable to maintain that degree of weight loss for a year, and that within two years more than half of what they had lost will be regained.
Unfortunately, scientists and medical doctors are still not sure of how best to lose unwanted weight to begin with and are even less sure about how to keep it off. We know that what we weigh is a matter of genetics, epigenetics (changes in the way that genes are expressed), and environment. Research has shown that our brains and our bodies play a vital role in both short-term regulation of calorie intake and long-term regulation of energy stores (fat).
Both sides of the energy equation—both energy intake and storage as well as energy expenditure from those stores—are monitored, however the monitoring system is somewhat lopsided. Our biology responds much more to weight loss than it does to weight gain, probably because evolutionarily, the threat posed by famine has been far more potentially dangerous than the threat posed by an overabundance of food. When we disturb the balance between food intake and energy expenditure, our bodies and our brains react.
We know that the brain monitors the availability of energy via circulating levels of hormones like leptin, ghrelin, Agouti-related protein or AgRP, and others. The actions of these hormones in the brain and body are widespread and complex. To put it as simply as possible, leptin is released by adipose tissue to signal the brain about how much fat (stored energy) is available. When plenty of energy is available, leptin levels are high and our appetites are low. Loss of adipose tissue when we successfully lose weight results in a decrease in the levels of leptin, signaling the brain to eat more and move around less. Ghrelin is a hormone produced and released in the gut. It signals the brain that the stomach is empty, encouraging us to eat. Ghrelin levels tend to increase as time since the last time we ate increases, and fall when we’re full. Ghrelin may be a short-term signal, letting the brain know that the tank is empty and we should refill it, while leptin may be acting more long-term, telling the brain about stored energy availability.

Both leptin and ghrelin interact with AgRP neurons in the brain, specifically in the hypothalamus. Leptin inhibits AgRP neurons in a part of the hypothalamus called the Arcuate nuclei (ARC) resulting in the suppression of appetite. Ghrelin also acts on the ARC AgRP neurons, stimulating them to release AgRP and resulting in an increase in appetite.
Grzelka, Wilhelms, Dodt, et al. (2023) examined the role of these hormones and their action in the hypothalamus and how they may be influencing the rebound in weight gain after successful weight loss. They found that weight loss in mice resulted in long-lasting strengthening of the synapses on the appetite-stimulating AgRP neurons of the hypothalamus. When the diet is over, and we’ve lost the weight, this long-term potentiation of the ARC cells might be part of the trigger to eat more. And that strengthening of the synapse resulting in increased release of AgRP is, as the name “long-term potentiation” implies, a long-lasting signal. They found that even a single activation of the synapse at the ARC cells resulted in a 10% increase in mouse body weight over the next week.
The good news may be that taking weight off and keeping it off can be done (success stories abound on the internet) and that yo-yo dieting, at least in mice, was not as bad for the mouse as simply staying obese (Engber, 2020). It seems that the best solution may be to not diet in the traditional sense at all. Instead, eating a healthy diet, getting some moderate exercise, and maybe not stressing about whether you’ve achieved runway model thinness may be just the ticket for a longer and happier life.
References
Martin, C.B., Herrick, K.A., Sarafrazi, N., and Ogden, C.L. (2018). Attempts to lose weight among adults in the United States, 2013-2018. Centers for Disease Control and Prevention, NCHS Data Brief No. 313, July 2018
Engber, Daniel (2020). Unexpected clues emerge about why diets fail. Scientific American, https://www.scientificamerican.com/article/unexpected-clues-emerge-abou…
Grzelka,K., Wilhelms,H., Dodt, S., Dreisow,M.-L., Madara, J.C., Walker, S.J., Wu, C., Wang, D., Lowell, B.B., and Fenselau, H. (2023). A synaptic amplifier of hunger for regaining body weight in the hypothalamus. Cell Metabolism 35, 1–16.


