Trauma
5 Myths About Trauma
Debunking some serious misconceptions about an increasingly popular concept.
Posted October 28, 2022 Reviewed by Davia Sills
Key points
- Trauma does not have to happen to you directly in order for you to experience its negative effects.
- Trauma doesn't have to change your brain forever—ample evidence shows that recovery from trauma is very real and very possible.
- Trauma itself is not a disorder; it is an adverse experience that may lead to a disorder.
- Resilience is the most common response to trauma.
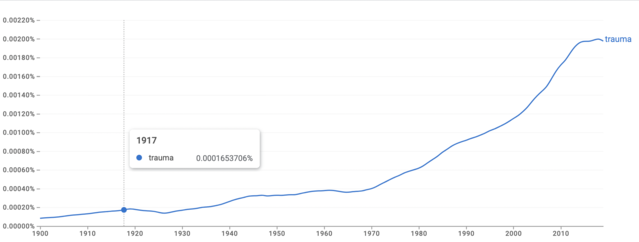
More people are talking about trauma than ever before. The number of articles and books published about the topic has grown substantially in recent decades. Over 5,500 podcast titles contain the word “trauma,” while the TikTok hashtag #Trauma alone has over 6.2 billion views. Social media engagement (likes, shares, reactions) ranks in the hundreds of thousands for posts mentioning “trauma,” and the term has skyrocketed in popularity as a Google search term.
Despite its increasing popularity as a topic, however, many people still hold some serious misconceptions about what trauma actually is. Here are five of the most pervasive myths about trauma—and what research has to say about them.
Myth: Trauma is a one-off horrific event that changes you forever.
An isolated event that severely violates a person’s physical and psychological safety can significantly alter that person’s mental (and physical) health. But trauma isn’t always a distinct and horrifying event. Many people’s experiences of trauma are chronic (think growing up in a chaotic living situation or being repeatedly exposed to domestic violence, residing in a community with high crime rates, or experiencing emotional neglect throughout childhood).
Trauma can also result from social and systemic factors like poverty and racism. Additionally, some research suggests that trauma can be transmitted from parents to offspring through mechanisms that influence DNA expression. Trauma is not, therefore, always a single event that changes you forever. It can manifest in different ways for different people, with vastly different outcomes and effects.
Myth: Trauma always leads to PTSD.
Post-traumatic stress disorder (PTSD) is a debilitating outcome of exposure to trauma(s) that entails intrusive and distressing memories of the traumatic event(s), avoidance of things associated with the traumatic event(s), impairments in memory and distorted thoughts or beliefs about one’s self or others (think: “I’m a bad person” or “Everyone’s out to get me”). Persistently depressed or agitated moods, feeling keyed up or on edge, and not being able to sleep or concentrate are other hallmarks of PTSD. So, too, is engaging in reckless or self-harming behavior.
Yet only a small proportion of people exposed to traumatic events (including the unexpected death of a loved one, violence, sexual assault, natural disasters, or vehicular accidents) develop PTSD. In fact, it’s estimated that just around six to eight percent of the population experiences PTSD symptoms during their lives. While we should never discount PTSD’s severity and risk factors, it’s important to remember that experiencing trauma does not always lead to PTSD.

Myth: Trauma is always a disorder.
Experiencing trauma can lead to or exacerbate a range of emotional, behavioral, and physical health issues. Disorders other than PTSD can result from trauma—including acute stress disorder, whose symptoms mirror those of PTSD but typically arise immediately after trauma exposure and last around one month; some personality disorders, eating disorders, anxiety, and depression. But this isn’t always the case. Many factors influence whether and how someone recovers from traumatic events, including their age at the time of the trauma, their personal coping skills and access to resources, what supports they have in place when trauma occurs, and whether they can access timely and effective interventions (like psychotherapy).
Approximately half of all people exposed to trauma actually go on to experience “post-traumatic growth”—a transformative and positive psychological experience in the wake of adversity that protects people from trauma’s negative effects. So while traumatic events can be life-altering or effect significant changes in one’s emotional and behavioral health, this isn’t the case for everyone exposed to trauma—nor is it true of every traumatic experience.
Myth: Trauma has to happen to you directly.
You don’t have to directly experience one or more traumatic incidents in order to be negatively affected by them. “Vicarious” or “secondary” trauma refers to a profound shift in one’s worldview and sense of safety resulting from repeated exposures to other people’s trauma—say, by witnessing the aftermath of disasters or hearing about vivid details of someone else’s adversity. Mental health professionals, health care professionals, emergency responders as well as clergy members who minister to people suffering from trauma’s effects are at higher risk of vicarious trauma than the general public.
Myth: Trauma changes your brain forever.
Experiencing trauma can alter our nervous system’s threat detection capacities, keeping us constantly on edge and on high alert for danger. But there’s evidence that our brains remain “plastic” (that is, changeable) well into the latter years of our life. Effective interventions for trauma—including eye movement desensitization and reprocessing (EMDR), modified versions of dialectical behavior therapy (DBT), and cognitive behavioral therapy (CBT)—have each been shown to change neural activity, bringing about positive emotional and behavioral changes observed in those who recover from trauma-related disorders.

The Takeaway
Not all experiences of trauma lead to disorders, and no two people’s responses to trauma are exactly alike. But even if your unique trauma response doesn’t meet the criteria for a disorder, that doesn’t mean you don’t need support processing and healing from what happened to you. And if your experience of trauma(s) has led to debilitating outcomes? All the more reason to seek help.
Recovery from trauma of all kinds is very possible—a reality that myths about trauma tend to obscure. With the right kind of support, trauma survivors can learn to regulate intense and overwhelming emotions resulting from past adversity, rekindle a sense of physical and emotional safety, develop trusting relationships with others, and extract meaning from their past so that it stops hijacking their present.
What happened to you doesn’t need to keep you a prisoner forever. You can and deserve to feel OK again. If you feel ready to take the step of reaching out to a therapist for support in healing from one or more traumatic experiences, don’t wait. You can look for a therapist near you on Psychology Today’s Therapist Directory.




