Empathy
A Patient's Need for That Empathic Witness
Writers reflect on their experiences as patients.
Updated April 3, 2024 Reviewed by Davia Sills
Key points
- Choosing a physician when symptomatic is difficult, for it is the first explicit confrontation with illness.
- Each person is ill in his own way, but all patients deserve a competent, attentive physician.
- Illness is a process that is made easier when a physician is a compassionate, empathic witness.
- Physicians have to titrate how much a patient wants to be involved in the decision-making.
“I flipped through the CT scan images, the diagnosis obvious: the lungs were matted with innumerable tumors, the spine deformed, a full lobe of the liver obliterated. Cancer, widely disseminated,” wrote 36-year-old neurosurgical resident Paul Kalanithi.
Over the six years of his training, Kalanithi had seen many such scans. He continued, “But this scan was different: it was my own.”
Kalanithi’s heartbreaking memoir, When Breath Becomes Air (2016), published posthumously by his wife, explored his valiant struggle: “Death may be a one-time event, but living with a terminal illness is a process.” Within 22 months from the time of diagnosis, Kalanithi would be dead.
With symptoms, including substantial weight loss and severe back pain for months, Kalanithi began to suspect the dreaded diagnosis; when test results confirmed his suspicions, he knew, as a physician, what lay ahead.

The experience of New York Times literary critic Anatole Broyard was very different. Though he had lived through the terminal illness of his father many years earlier, Broyard described himself, at age 69, as having had almost no relationship with doctors and felt like a “mere beginner” as a patient. Diagnosed with prostate cancer, he was dead within 14 months.
Written almost 35 years ago, Broyard’s book, Intoxicated by My Illness, can still serve as a template for the expectations patients may have of their physicians and what it is like to experience thoughts about their mortality.
“To the typical physician, my illness is a routine incident in his rounds, while for me, it’s the crisis of my life. I would feel better if I had a doctor who at least perceived this incongruity,” wrote Broyard. He wanted not only a talented physician but a “bit of a metaphysician, too. Someone who can treat body and soul.”
Broyard described difficulties in choosing a doctor because it is the “first explicit confrontation with our illness.” Like Tolstoy’s first line of Anna Karenina, “…each unhappy family is unhappy in its own way,” Broyard acknowledged that each person is ill in his or her own way.
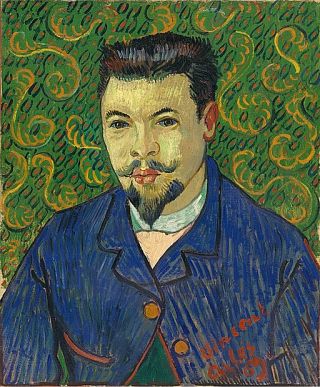
A physician, at least for him, should have style and “should be able to imagine the aloneness of the critically ill, a solitude as haunting as a de Chirico painting.” Broyard’s ideal physician understands the concept of empathic witnessing.

Empathic witnessing is somewhat analogous to Robert Louis Stevenson’s concept of a life witness. Stevenson, who gave us Treasure Island, A Child’s Garden of Verses, and Dr. Jekyll and Mr. Hyde, wrote in one of his essays that by marrying, “You have willfully introduced a witness into your life” (1881; Karasu and Karasu, 2005). A physician, in other words, in the best of circumstances, can also become that special compassionate partner or observer—that witness—who experiences the process of illness together with the patient.
Though well-schooled in the language of illness, Kalanithi came to understand the “physician’s duty is not to stave off death or return patients to their old lives,” but to embrace both patients and their families “whose lives have disintegrated…” He continued, “What patients need is not scientific knowledge... but existential authenticity… the angst of facing mortality has no remedy in probability.”
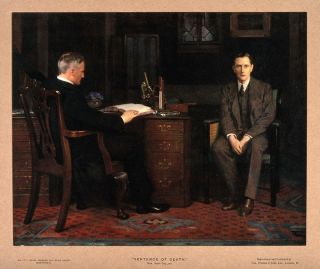
Unfortunately, though, there are those physicians who don’t observe. Broyard described physicians who “give you a generic, unfocused gaze. They look at you panoramically. They don’t see you in focus... and you are a figure in the ground.” When a doctor fails to acknowledge a patient, the doctor is, in effect, “abandoning” the patient to his or her illness.
Such was the experience of historian, author, and Yale professor Timothy Snyder, who poignantly described his excruciating visit to one Connecticut emergency room. “The doctors and nurses could not spend more than a few seconds at a time with me,” and looking down at their computer screens, they rarely made eye contact. Their cell phones rang, causing one physician to startle in the middle of performing a delicate (and ultimately unnecessary) spinal tap on Synder. “My body was at the mercy of the permanent distraction of doctors” (Snyder, 2020).
Not only does a patient want an attentive, genuinely concerned, and competent physician, but one who listens. Subtleties in communication can make a considerable difference.
For example, “Is there anything else?” conveys more of a negative feeling than “Is there something else?” (Mikesell, 2013). Further, physicians may seem insensitive when using language such that patients interpret “treatment failure” or “failing” chemotherapy as if they had failed rather than the chemotherapy failed them (Dizon et al.).
Other insensitivities or inadequacies in physician responses to patients include interrupting, avoiding, or discouraging discussion about emotional concerns, inadequate acknowledgment of or even overt denial of concerns, and use of thoughtless humor. A patient’s agenda may conflict with the physician’s agenda (Zimmermann et al., 2007).
Broyard suggested that part of the problem may lie with the hospital atmosphere itself: The hospital “ought to be less like a laboratory and more like a theater, which would be fitting since no place contains more drama.” He appreciated that the laboratory atmosphere may have originated in the avoidance of contagion: “The patient was protected by the sterility of the hospital.”
But, continued Broyard, “The sterility went too far: It sterilized the doctor’s thinking” and the patient’s entire hospital experience. “It sterilized the very notion of illness to the point where we can’t bring our soiled thoughts to bear on it.”
“Soiled thoughts” aside, patients may need more of a “delicate balance” between hearing too much and hearing too little information: They can fixate on a detail that may be irrelevant to their treatment. In recent years, and particularly with the extensive information available on the internet, patients often want greater involvement in their care. Physicians, though, should not assume that patients necessarily want full control (Dizon et al., 2013).

For example, as a physician, Kalanithi had been intimately involved in decision-making with his oncologist. At one point, that burden seemed particularly great, and the oncologist suggested that she could just be the doctor. “I had not even considered that I could release myself from the responsibility of my own medical care,” he wrote.
During his ordeal, Kalanithi was fortunate to have an oncologist who was a caring, attentive, and empathic witness, but when she told him he had five good years left, “she pronounced it without the authoritative tone of an oracle” or the “confidence of a true believer.” She said it, instead, “like a plea.” Doctors, Kalanithi realized, “need hope too.”
The experiences of these three writers—Broyard, Kalanithi, and Snyder—span almost 35 years, during which time, extraordinary innovations have occurred in medicine. Unfortunately, the angst of confronting mortality and the importance of the physician as an empathic witness have remained and are sometimes made worse by the complexities of our healthcare system and the burdens placed on both physicians and patients.
References
Broyard A. (1992). Intoxicated by My Illness and other Writings on Life and Death. New York: A Fawcett Columbine Book Published by Ballantine Books.
Dizon DS et al (2013). The power of words: discussing decision making and prognosis. American Society of Clinical Oncology Educational Book: 442-446.
Hirshler EE. (2023). Fashioned by Sargent. (Comments on Dr. Samuel Pozzi). Boston: Museum of Fine Arts, Boston.
Kalanithi P. (2016). When Breath Becomes Air. New York: Random House, an imprint and division of Penguin Random House LLC.
Karasu SR; Karasu TB. (2005). The Art of Marriage Maintenance. Lanham, Maryland: Rowman and Littlefield Publishers, Inc.
Mikesell L. (2013). Medicinal relationships: caring conversation. Medical Education 47: 443-452.
Snyder T. (2020). Our Malady: Lessons in Liberty from a Hospital Diary. New York: Crown, in imprint of Random House, a division of Penguin.
Stevenson, RL. (1881). Virginibus Puerisque and Other Papers. Harmondsworth. Reprint, London: Penguin (1949), pp. 25-26.
Tolstoy L. (2004) Anna Karenina. Translated by Richard Pevear and Larissa Volokhonsky. New York: Penguin Classics, Deluxe Edition.
Zimmermann C; Del Piccolo L. (2007). Cues and concerns by patients in medical consultations: a literature review. Psychological Bulletin 133(3): 438-463.




