SSRIs
Safer Tapering to End Antidepressant Treatment
An offramp from antidepressants.
Posted November 2, 2022 Reviewed by Lybi Ma
Key points
- Antidepressant use has increased worldwide, with insufficient attention on how to stop treatment that is no longer needed.
- Few guidelines and resources are available, and prescribers are unable to provide adequate support.
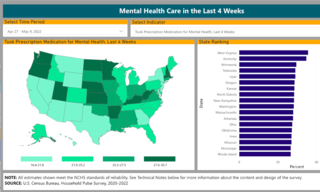
Close to 3.4 million Canadians and more than 1 in 7 Americans take antidepressants, and their usage worldwide has increased significantly in recent years. Among OECD countries, according to 2021 data, Iceland and Portugal record the highest use, at 146 and 124 people per 1,000. But in the U.S., where per capita use is even higher, the percentage of adults taking an antidepressant the previous month rose to 23.1 percent this year. West Virginia, Kentucky, and Minnesota all recorded use above 30 percent.
In anticipation of World Tapering Day— November 5—a company headquartered in Toronto, Ontario, and soon to open in the U.S., is starting “the world’s first comprehensive, personalized, and evidence-based platform to help people safely reduce or stop antidepressants when they are no longer needed.”
The company—called Outro, to emphasize the desired exit from antidepressant treatment—draws from a team of experts on antidepressant tapering and withdrawal, in alignment with prescribers and pharmacies—to provide individualized protocols for tapering and titration. This includes proactive symptom monitoring, one-on-one chats and video appointments with trained practitioners, and a patient-first approach that minimizes relapse risks while maximizing the chances of success.
“We follow the approach that has recently been established as best practice in Britain,” explains Dr. Mark Horowitz, a Clinical Research Fellow in Psychiatry in the UK’s National Health Service, “as outlined by the Royal College of Psychiatrists in their guidance on ‘stopping antidepressants.’” A contributing author to that guidance, Horowitz, whose Lancet publication “Tapering of SSRI treatment to mitigate withdrawal symptoms” similarly informed national guidance by the UK’s health and medicines watchdog, is one of the company’s founders.
Also informing the guidance are the experiences of patient advocate and Outro team member Adele Framer, whose article, “What I have learned from helping thousands of people taper off antidepressants and other psychotropic medications,” has been downloaded more than 96,000 times since publication in March 2021.
Outro’s patient guidance stems from the awareness that a substantial number of people have been on antidepressants longer than is typically recommended. According to CDC data, even before COVID-19 two-thirds of U.S. patients had taken antidepressants for more than two years, and one-quarter for longer than 10 years.
Integral to company policy is an understanding that coming off antidepressants is a complex process, frequently more difficult than reported. Many prescribers are unable to provide guidance or support, leaving patients unsure of where to turn and how best to proceed.
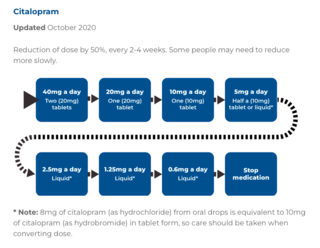
Tapering—or, in liquid form, titrating—“ultra slowly” over months reduces the intensity of withdrawal symptoms and gives time for the brain to adapt to the lower levels of the drug. A pattern can be established concerning the rate of reduction an individual can tolerate, tied as much to their medication history, age, and physiology as to the symptoms that led them to seek treatment.
Given the few tapering resources available to patients across North America, I asked the company founders what guidance and support a client could expect with their personalized protocol. Their answer:
- Initial assessment of the patient by trained clinical staff to determine if stopping an antidepressant is the right clinical decision for them. Assessment is based on the history of their condition, current circumstances, treatment history, and the harms and benefits of their current treatment.
- Education about the process of closely monitored, gradual tapering according to a hyperbolic pattern, including the rationale for this approach.
- Education about what withdrawal symptoms are, why they occur, and what the approach to them will be: if they are too severe, pausing the reduction or going back up, waiting for symptoms to resolve, and then tapering at a more gradual pace.
- An estimation of each person’s risk of withdrawal based on their medication use.
- A first reduction is agreed upon, based on an estimate of risk and shared decision-making.
- The patient monitors their symptoms using a digital platform that communicates with their clinician. If there are any issues they can contact their clinician directly.
- Further reductions are made according to the response to this reduction. The process is repeated until the medication is stopped.
When I followed up by asking exactly how the data-driven design would lower the risks of excessive dosage reduction, the answer was similarly detailed, concluding:
“The hyperbolic [i.e., ultra slow] tapering method Outro uses places significant emphasis on careful monitoring of symptoms, high responsiveness to increasing withdrawal symptoms, and careful titration of the rate of reduction based on symptoms, all in the context of easily accessible support from experts trained by leaders in the field. In this way, excessively quick dose reductions are avoided.”
“Although things are slowly changing in Britain,” Horowitz summed up to me, regarding antidepressant withdrawal guidelines and protocols for safer tapering, “in North America people are still pouring into Facebook groups and onto peer-support websites in search of guidance they can’t get from their doctors on how to safely get off antidepressants. We thought this was an absurd situation and decided to set up a professional medical service to fill the unmet need."


