SSRIs
Pandemic Prescribing of Antidepressants
Global increase in SSRI use raises concerns about safety, environmental impact.
Posted April 7, 2022 Reviewed by Michelle Quirk
Key points
- Poor mental health during the pandemic may occur in the context of family economic impacts, caregiving needs, hunger, and abuse in the home.
- Between 1991 and 2018, total SSRI consumption increased in the United States by 3001 percent.
- Most wastewater treatment plants lack the requisite removal methods to eliminate traces of SSRIs from drinking water.

With the publication of significant new data, a clearer and fuller picture is starting to emerge about selective serotonin reuptake inhibitor (SSRI) prescribing both before and during the past two years. We also have useful granular data on the toll the pandemic has taken on individual and collective mental health.
Among the factors needing careful assessment is the cost of the sharply increased prescribing on persons, bodies, budgets, and the environment, relative to its stated benefits. With the environment, so often overlooked by researchers, concern centers on the impact of large traces of SSRI antidepressants on the soil, subsoil, and surface waters used for drinking water, with treatment plants worldwide that normally “do not have the necessary removal methods to eliminate these pharmaceuticals.”
Increases in SSRI Use Around the World
In the latest issue of Science of the Total Environment, five colleagues in toxicology and chemistry at Mexico’s Universidad Autónoma de Estado de México, led by professor Nidya Diaz-Camal, compare prescribing rates for SSRI antidepressants both before and during the COVID-19 pandemic and conclude that “worldwide consumption of antidepressants increased significantly during the pandemic.” As a result of that rise, “concentrations of SSRIs in the environment increased” as well.
Between 1991 and 2018, they note, the “total consumption of SSRIs increased by 3001% in the United States,” from $64.5 million in 1991 to $2 billion by 2004, before dipping to $755 million in 2018. Closer analysis of the Medicaid program they cite shows that the “total number of antidepressant prescriptions increased substantially” between 1991 and 2004, from 6.8 million scripts to 35 million, more than a 400 percent increase, as SSRIs “gradually came to dominate the market over the last 15 years.”
Studies of Organisation for Economic Co-operation and Development countries in Europe report smaller but still substantial percentage increases over a similar period, with the consumption of antidepressants found to double between the years 2000 and 2019, “making European countries the largest consumers of antidepressants in the world.”
More recent, granular data since the start of the pandemic draw from a 2020 study in England that found an additional 92 million units of antidepressants prescribed between January and August 2020, a relative increase of 5.78 percent over the same period the previous year.
A two- to threefold increase in antidepressant prescribing was found to exist across France, the United Kingdom, the United States, Asia, and Australia more generally, though in the United States in February and March 2020 “a 21% increase in the number of antidepressant prescriptions was observed,” making those months “the highest since the declaration of the Covid-19 pandemic” at the start of the year.
Increased Stress, Anxiety, and Depression
The data on increased SSRI consumption aligns broadly, if imperfectly, with higher levels of recorded stress in most of the same countries. Studies conducted in Germany and Italy early in the pandemic found that 7.2 percent of the participants had severe anxiety, 11.5 percent had very severe anxiety, 12.6 percent had very severe stress symptoms, and 15.4 percent had very severe depression.” Northern Italy was among the regions first and hardest hit by the first wave of coronavirus.
Recent data from the United States—including the Centers for Disease Control and Prevention’s 2021 Adolescent Behaviors and Experiences survey, published earlier this month—report similar steep declines in teen mental health, with more than one in three high-school students experiencing poor mental health during the pandemic and nearly half of students (44.2 percent) over the preceding 12 months reporting persistent feelings of sadness or hopelessness. In addition, 19.9 percent had seriously considered attempting suicide, and 9.0 percent had attempted suicide.
The factors influencing these findings were both specific and wide-ranging and included difficulties such as family economic impacts, hunger, and abuse in the home. More than half (55 percent) reported emotional abuse from an adult in their home, and 11 percent reported physical abuse from an adult at home. Roughly a third (29 percent) reported that an adult in their home had lost a job due to the pandemic.
The anxiety, stress, and depression that may appear as relatively straightforward drivers of increased SSRI prescribing are thus shown to arise in a context of reports of widespread emotional and physical abuse, heightened job loss and insecurity, and sharply higher stress over COVID-19–related caregiving and mitigation, among them the consequences of living with long COVID. Diaz-Camal and colleagues also recorded in their meta-study increased reports of disorientation and confusion, memory impairment, posttraumatic stress disorder, and insomnia.
In addition to concerns about their modest efficacy relative to placebo, SSRIs introduce problems of their own. “Associated with increased hostility, suicidal ideation, and psychomotor agitation in clinical trials with children, adolescents, and young adults,” they are frequently associated with sexual dysfunction and long-lasting withdrawal symptoms, and for the body and environment generate problems because they do not metabolize rapidly or straightforwardly. As a result, Diaz-Camal and colleagues warn that the “increase in antidepressant use worldwide raises concern about the safety, efficacy, and environmental impact of long-term use.”
SSRIs in the Water
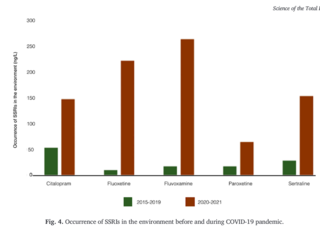
From toxicology reports of SSRIs on diverse aquatic organisms, principally fish, and studies of the drugs’ “unchanged metabolites” on “discharges of industrial, domestic, and hospital effluents,” the researchers find such recurring traits in the fish as “significant decrease in locomotor activity,” “significantly lower velocity,” “reduction of swimming distance,” and “increased aggression.” In the case of fluoxetine (Prozac), under “affects sexes differentially,” they note “altered male mating strategy” and “affected maturation of predatory behavior,” including “significantly more coercive ‘sneak’ copulations,” and the drug “affecting the [species’] total hatching time,” by accelerating it.
The most-effective method for removing citalopram from drinking water, we learn, is “by photolysis,” whereas “for fluoxetine it is electron beam irradiation, for paroxetine it is printed molecular polymers, and for sertraline it is photolysis and printed molecular polymers.”
In short, ridding our drinking water of SSRI metabolites—exactly the kind prescribed in record numbers worldwide—has “become a new opportunity era” for water-treatment plants.
Let us hope that the financial incentives prompt fast action. Currently, SSRIs are not included on the watchlists regulated by the Water Framework Directive of the European Commission, and “most wastewater treatment plants do not have the necessary removal methods to eliminate these pharmaceuticals.”
Until action is taken, the trace elements of mass-prescribed antidepressants will remain “widely distributed in surface waters around the world,” to varying degrees, altering the behavior of every animal and human that comes into contact with them.
As one of the researchers, Hariz Islas Flores, put it when I reached out for comment, “The monitoring of environmental concentrations [of SSRIs], as well as the development of new technologies that allow for the removal of this contaminant (without the generation of even more toxic waste) is of the utmost importance, due to the amount of toxic effects they produce in nontarget organisms.”
References
CDC: Centers for Disease Control and Prevention (April 2022). 2001 Adolescent Behaviors and Experiences Survey (ABES). [Link]
Diaz-Camal N, Cardoso-Vera JD, Islas-Flores H, Gómez-Oliván LM, Mejía-García A. Consumption and occurrence of antidepressants (SSRIs) in pre- and post-COVID-19 pandemic, their environmental impact and innovative removal methods: A review. Sci Total Environ. 2022 Mar 19;829:154656. doi: 10.1016/j.scitotenv.2022.154656. Epub ahead of print. PMID: 35318057. [Link]




