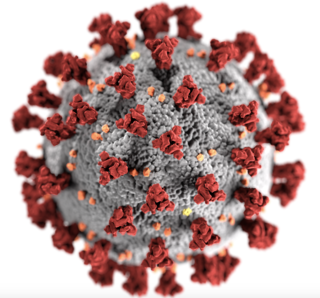
Coronavirus Disease 2019
6 Reasons Why COVID-19 Is Nothing Like the Flu
The constant comparisons with the flu are wrong and harmful.
Posted May 6, 2020 Reviewed by Gary Drevitch
By now, you've probably encountered commentary likening the COVID-19 pandemic to the seasonal flu. Sometimes it's about the numbers affected by the two diseases, and sometimes it's about the actual illness, symptoms, and outcomes. On a post about my own COVID-19 recovery, an acquaintance wrote, "Sounds like you had a bad case of the flu." Um, no. Not at all. On another post, someone wrote simply, "Flu kills more." Also no.
COVID-19 and the flu are very different conditions and the two viruses that cause them, SARS-CoV-2 and influenza a or b, respectively, have little in common. The comparisons are not only inaccurate, they're dangerous, almost always meant to minimize the threat posed by one of the most dangerous contagions we've ever faced.
This is the first of a two-part series discussing some of the ways these two deadly diseases are totally different. Below, I focus on the clinical differences. In part two, I focus on the molecular differences.
Symptoms. The seasonal flu and COVID-19 have very different symptomatologies. Both usually involve a cough, sore throat, and fever, but these present differently. For example, the flu causes chest congestion, the cough is "productive," and there are also upper respiratory (nasal) symptoms such as sneezing and runny nose. With COVID-19, there are usually no nasal symptoms, the cough is often dry, and there isn't a lot of mucus in general (whereas mucus is the hallmark of the flu). Headaches, body aches, and fatigue are also common to both, but those are felt in essentially all infections, as these are side effects of immune system proteins called cytokines. COVID-19 also involves poor oxygen delivery and shortness of breath, and, bizarrely, loss of taste and smell. These are not common symptoms of the flu.

Severity and duration. In addition to having different symptoms, COVID-19 illness is often more debilitating than the flu and it lasts much longer, on average. While the flu tends to last 5-10 days, cases of COVID-19 are measured in weeks. I was sick for three weeks, longer than I've ever been ill with the flu or anything else. A work colleague of mine has been sick for two full months. Our babysitter has been sick for six weeks and was hospitalized twice for several days each. My uncle has been in the hospital, in and out of the ICU, for five weeks (UPDATE: He passed away). Another work colleague was sick for a week before being admitted to the hospital and spending nearly three weeks in the ICU before finally losing his battle.
Mortality. This is a tough issue because we don't yet have solid metrics for COVID-19. Some countries like Belgium have reported that 15% of cases are lethal, while the U.S. mortality rate hovers between 2 and 5%. But these numbers reflect the fact that only the most severe cases were being tested until recently. The true mortality rate appears to be just below 1%, but is much higher in those with co-morbidities such as obesity, hypertension, diabetes, congestive heart disease, asthma, cancer, kidney failure, etc., and that's a lot of people, especially in the U.S. The mortality rate begins to jump at around age 70, killing 10-15% of those in their eighth decade. For those above age 80, more than 20% who fall ill will die, dwarfing the mortality rate of influenza.
In the last 10 years of seasonal flu, the mortality rate has never breached 1%, even in the 65-plus age group. In sum, COVID-19 is more lethal than the flu across all age groups but is 10 to 20 times more lethal in the elderly. I haven't personally known anyone who died of influenza, but I know five people who have died of COVID-19 in the past two months (including a cousin in his early 50s and previously in perfect health).

Contagiousness. How fast an infectious disease can spread through a population is an important factor for understanding its danger, but this metric is a moving target, especially when precautions are in place to reduce the spread we're trying to measure. Epidemiologists measure a disease's ability to spread using something called the "Basic Reproduction Number" (BRN), which is akin to the number of future cases that each new case will infect while the disease is spreading unchecked. For the past 10 years or so, the BRN for seasonal flu has been between 1 and 2. Contagious, but manageable. During the 2009 flu pandemic, the BRN was nearly 2. During the global influenza pandemic of 1918, the BRN was 2.8. Most measurements for COVID-19 are between 3 and 5, making it more contagious than SARS, Ebola, and Smallpox (but less so than Measles, Mumps, and Chickenpox).
Demographics. Much has been made of the age preference of SARS-CoV-2 by those wishing to minimize its dangers. While it is true that this virus preys most intensely on the elderly and those with underlying health conditions, that is true of literally every infectious disease, because the effectiveness of our immune system wanes with age and is hampered by certain co-morbities. Not to get lost in this discussion is the shocking number of otherwise healthy people in their 30s, 40s, and 50s who have become critically ill with COVID-19. I've had the flu before and never missed more than a couple days of work. I'm 41 and COVID sickened me for three weeks.
Long-term disability. It is tempting to think that COVID-19 is like the flu or a cold in that, once you recover from it, you are exactly as you were before. But there are many viruses that leave patients with long-term disabilities. Polio patients remain paralyzed long after the virus has been cleared. Many patients with bad cases of West Nile virus develop Parkinsonian tremors, neurodegeneration, and other cognitive impairments. Even chickenpox can lead to painful shingles for years to come, due to the reactivation of dormant viruses within sensory neurons. Since it is so new, we don't yet have the full picture of long-term problems COVID-19 might leave in its wake, but the early signs are ominous.
Blood clots, including lethal pulmonary embolisms, are now a recognized complication of COVID-19. On a likely related note, hospitals around the world are reporting a startling number of strokes in otherwise healthy patients in their 30s and 40s suffering from a mild or asymptomatic case of COVID. The virus has also been shown to cause permanent liver damage in some patients. Remember the loss of taste and smell? That's a neurological symptom (!), one of several that COVID-19 can cause including confusion, seizures, and even brain damage. COVID-19 wreaks havoc throughout the body and can lead to a condition called multiple organ failure, which is as devastating as it sounds.
We also know that many recovered COVID-19 patients (including yours truly) have persistent joint pain and those with rheumatoid arthritis report lasting flare-ups of their symptoms. This is likely due to the exaggerated immune response, but what remains to be seen is whether the joint damage is permanent or just stubborn. The point is that we are just starting to learn of the systemic damage the virus causes throughout the human body, something we don't often see with influenza.
COVID-19 and the flu are entirely different illnesses. Aside from some overlapping symptoms and tendency to spread all over the globe, they are not readily comparable. The reason they present such distinct challenges is that they are caused by very different viruses, as I explain in part two.




