A Bug in the System
Susceptibility to psychiatric disorders may be set by gut bacteria.
By Hara Estroff Marano published May 2, 2017 - last reviewed on July 3, 2017
It's becoming an axiom of medicine: "You can't have a healthy mind without a healthy gut," as Timothy G. Dinan, one of the world's foremost researchers on the microbiome puts it. Actually, you can't have a healthy anything without a healthy gut. In many ways still not fully understood, the gut influences the integrity of the immune system, metabolism, cardiovascular function, to name just a few systems.
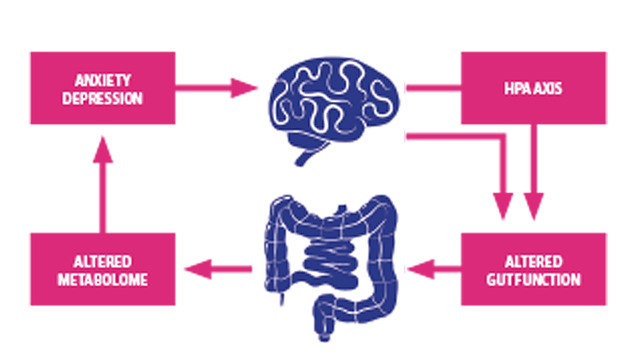
As for the mind, maintain the best troops among the vast army of bacteria in the gut and you can resist stress and related disorders such as depression and anxiety, says Dinan, of Ireland's University College Cork. The body's response to stress intrinsically involves the gut microbiome. Hormones released by the brain's hypothalmic-pituitary-adrenal axis in response to the perception of threat prepare the body to meet a challenge or flee from it. An array of changes occurs quickly, including the way the gut functions. One result, Dinan finds, is an alteration in the diversity of the gut bacteria.
In addition to influencing daily functioning, there is also growing evidence that there are particular "windows" during development of the nervous system when its very threshold of responsiveness is set by the diversity of bacteria that make up the microbiome. Those periods—pre- and perinatal development and again at adolescence—may be especially critical in creating susceptibility to or resilience to stress throughout the lifetime.
The microbiome not only seems to set the level of stress susceptibility, it also plays a role in learning, researchers find. Specific strains of gut bacteria influence fear learning and extinction, processes dependent on the amygdala and central to anxiety conditions such as PTSD. The research raises the possibility of engineering stress resistance, especially in soldiers, through a probiotic-rich diet.
When Dinan and colleagues supplied the probiotic Bifidobacterium longum 1714 to 22 healthy male volunteers for a month and subjected them to a specific challenge, they found reduced levels of stress measured psychologically and physiologically. The researchers recorded improvements in visuospatial memory as well as a blunted hormonal response to stress.
The bacterial composition of the microbiome may also be responsible for much of the ebb and flow of symptoms in such psychiatric conditions as bipolar disorder and schizophrenia. Researchers at Johns Hopkins, for example, have found a more than fivefold increase in manic episodes among psychiatric patients taking antibiotics.
There is a direct channel of communication between the gut and the brain via the vagus nerve, and gut bacteria produce specific neural signaling molecules by which messages are transmitted to the brain, influencing mood and cognition. But gut bacteria also produce important metabolites and lipids that regulate brain function.
Antibiotic treatment of infection, consumption of a poor diet, and stress have all been shown to disrupt composition of the gut bacteria, affecting the substances such bacteria produce and the signals they send. But it may be that diet, antibiotics, and stress also change the function of the gut in ways that activate immune cells, which, by stirring inflammation in the brain, induces psychiatric symptoms.
Adolescence is a period when brain connectivity undergoes major change. It is also a time when many psychiatric disorders first appear. According to neurovirologist Robert Yolken, adolescents may be especially susceptible to the psychiatric effects of gut-bacteria shifts resulting from antibiotic use. Infection prevention and control, in fact, may be the next frontier of mental illness treatment.
The use of probiotics to restore bacterial balance is already under study as a treatment for psychiatric conditions. Yolken and colleagues are now testing whether probiotic treatment reduces the occurrence of manic episodes in those with bipolar disorder.
It's becoming an axiom of medicine: "You can't have a healthy mind without a healthy gut," as Timothy G. Dinan, one of the world's foremost researchers on the microbiome puts it. Actually, you can't have a healthy anything without a healthy gut. In many ways still not fully understood, the gut influences the integrity of the immune system, metabolism, cardiovascular function, to name just a few systems.
As for the mind, maintain the best troops among the vast army of bacteria in the gut and you can resist stress and related disorders such as depression and anxiety, says Dinan, of Ireland's University College Cork. The body's response to stress intrinsically involves the gut microbiome. Hormones released by the brain's hypothalmic-pituitary-adrenal axis in response to the perception of threat prepare the body to meet a challenge or flee from it. An array of changes occurs quickly, including the way the gut functions. One result, Dinan finds, is an alteration in the diversity of the gut bacteria.
In addition to influencing daily functioning, there is also growing evidence that there are particular "windows" during development of the nervous system when its very threshold of responsiveness is set by the diversity of bacteria that make up the microbiome. Those periods—pre- and perinatal development and again at adolescence—may be especially critical in creating susceptibility to or resilience to stress throughout the lifetime.
The microbiome not only seems to set the level of stress susceptibility, it also plays a role in learning, researchers find. Specific strains of gut bacteria influence fear learning and extinction, processes dependent on the amygdala and central to anxiety conditions such as PTSD. The research raises the possibility of engineering stress resistance, especially in soldiers, through a probiotic-rich diet.
When Dinan and colleagues supplied the probiotic Bifidobacterium longum 1714 to 22 healthy male volunteers for a month and subjected them to a specific challenge, they found reduced levels of stress measured psychologically and physiologically. The researchers recorded improvements in visuospatial memory as well as a blunted hormonal response to stress.
The bacterial composition of the microbiome may also be responsible for much of the ebb and flow of symptoms in such psychiatric conditions as bipolar disorder and schizophrenia. Researchers at Johns Hopkins, for example, have found a more than fivefold increase in manic episodes among psychiatric patients taking antibiotics.
There is a direct channel of communication between the gut and the brain via the vagus nerve, and gut bacteria produce specific neural signaling molecules by which messages are transmitted to the brain, influencing mood and cognition. But gut bacteria also produce important metabolites and lipids that regulate brain function.
Antibiotic treatment of infection, consumption of a poor diet, and stress have all been shown to disrupt composition of the gut bacteria, affecting the substances such bacteria produce and the signals they send. But it may be that diet, antibiotics, and stress also change the function of the gut in ways that activate immune cells, which, by stirring inflammation in the brain, induces psychiatric symptoms.
Adolescence is a period when brain connectivity undergoes major change. It is also a time when many psychiatric disorders first appear. According to neurovirologist Robert Yolken, adolescents may be especially susceptible to the psychiatric effects of gut-bacteria shifts resulting from antibiotic use. Infection prevention and control, in fact, may be the next frontier of mental illness treatment.
The use of probiotics to restore bacterial balance is already under study as a treatment for psychiatric conditions. Yolken and colleagues are now testing whether probiotic treatment reduces the occurrence of manic episodes in those with bipolar disorder.
Stress Cycles
Facts of (Bacterial) Life
- Antibiotics used anywhere in or on the body disrupt the makeup of the biome.
- Germ-free mice have an exaggerated hormonal response to stress.
- The standard Western diet, high in saturated fat and sugar, significantly affects the composition of gut bacteria in ways that promote neuroinflammation and cognitive dysfunction.
- Prenatal stress diminishes the diversity of the infant microbiome.
- Childbirth by cesarean section may alter composition of the infant biome to lastingly affect stress responsiveness.
- Gut bacteria transferred from patients with major depression to animals also transfer depressive-like behaviors to the animals.
- Parkinson's disease has been linked to changes in the microbiome.
- Consuming prebiotics and probiotics during puberty may confer stress resilience and prevent the development of psychiatric disorders.
- The best "smart drug" may be a probiotic; boosting the microbiome also boosts learning and memory.
- Specific strains of bifidobacteria and lactobacilli are most linked to positive effects on brain and behavior.
