Eating Disorders
"What Hath Night to Do with Sleep?" Night Eating Syndrome
The controversies about making a diagnosis of an eating disorder
Posted January 25, 2014
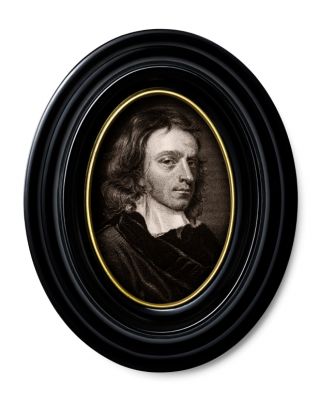
The 17th Century English poet John Milton (famed for Paradise Lost) wrote a play/poem popularly called Comus, after Komos, the Greek mythological god of nighttime festivities and excesses of all kinds. In his work, technically called a “mask,” (an elaborate musical performance) Milton tells the story of three siblings traveling through a forest at night. The sister, who becomes separated from her brothers, comes across a disguised and treacherous Comus (son of Bacchus and Circe) who tries to seduce her with an intoxicating potion and tempting food--“lickerish baits”..."all manner of deliciousness...tables spread with all dainties” as he claims he can reunite her with her brothers. Says Comus, “What hath night to do with sleep?”
Those English scholars among you appreciate that Milton’s poem of self-control and self-indulgence is about much more than nighttime eating and revelry. (There has been the suggestion that Milton’s work was loosely based on an actual legal case of rape.) Comus’s line, though, provides a metaphor for those who are tempted by Milton’s description of “swinish gluttony” to eat most of their food at night--those who have the so-called night eating syndrome--and for some, have an increased risk of obesity.
Originally described in the mid-1950s by psychiatrist and major researcher in the field, Albert J. Stunkard, M.D., the night eating syndrome consisted of three distinct characteristics: nocturnal hyperphagia, insomnia, and morning anorexia (i.e., negligible interest in eating breakfast.) Stunkard initially believed that the clinical syndrome developed in the context of psychological stress and often led to “untoward reactions to dieting,” such as depression and anxiety, as well as obesity.
Over the years since Stunkard’s initial description, studies in the literature have used somewhat different and

inconsistent criteria. There was apparently considerable discussion and controversy during preparation of the fifth edition of the Diagnostic and Statistical Manual of Mental Diseases (DSM-5) on whether to include the night eating syndrome as a psychiatric diagnosis for this very reason. While binge-eating disorder has now been included, ultimately, the panel for Eating Disorders for DSM-5 opted not to include the night eating syndrome in this edition of the Manual. For those interested in a more in depth discussion, see the review article by psychologist Ruth Striegel-Moore, a member of the Panel, and her colleagues, including the options they had considered for inclusion in DSM-5 in their 2009 article in the International Journal of Eating Disorders. Their review found “significant limitations and gaps in the scientific literature of the night eating syndrome.” They also noted that earlier reports focused on overeating while more recent reports have focused on the timing (i.e. nighttime) of the eating. Furthermore, Striegel and her colleagues could not find consistent support for the notion that night eating (rather than excessive caloric intake) necessarily leads to weight gain or obesity.
Stunkard and his group, including Dr. Kelly C. Allison, at the University of Pennsylvania School of Medicine, have been at odds with Striegel-Moore and her colleagues. They had recommended that the night eating syndrome be included as an eating disorder in DSM-5 and have proposed the following constellation of symptoms: daily pattern of eating demonstrates at least 25% of food intake is consumed after the evening meal for at least two or more days a week; awareness and recall of the eating episodes (as different, for example, from reports of eating that are not recalled when taking the sleeping medication Ambien); and a clinical picture characterized by three of the following: negligible interest in eating breakfast (i.e., early morning anorexia) at least four or more mornings a week; presence of a strong urge to eat after dinner and during the night; presence of a belief that one must eat in order to return to sleep; and depressed mood that is worse in the evening. Furthermore, this disordered eating pattern is associated with significant distress, has been maintained for at least three months, and is not secondary to a medical condition or substance use disorder or other psychiatric illness. For a more complete discussion of their criteria, see the article by KC Allison et al in the 2010 International Journal of Eating Disorders.
Vander Wal, in a critical review of the literature, in a 2012 article in the journal Clinical Psychology Review, believes that the night eating syndrome is associated with obesity. Vander Wal also noted that it appears to run in families, may involve the neurotransmitter serotonin, as well as involve a circadian rhythm “dysregulation” of certain hormones such as leptin and melatonin. Medications such as the selective serotonin reuptake inhibitors (SSRIs), (e.g., sertraline-Zoloft) have been used with some effect, as has bright light therapy, and cognitive behavioral therapy. Along those lines, Kucukgoncu et al, in a cross-sectional study at Yale University’s Department of Psychiatry, report in the recent 2014 article in European Eating Disorders Review, that the night eating syndrome was seen in over 21% of 155 patients with major depression, as diagnosed by the criteria proposed in that 2010 article by KC Allison and her colleagues. Their conclusion was that the night eating syndrome was common and was associated with increased weight (significantly higher body mass index--BMI) (and increased food intake) as well as with smoking and should be “carefully evaluated” by clinicians for their depressed patients.
Bottom line: The night eating syndrome has suffered from a lack of consistent criteria until more recently and as a result, unfortunately was not included as an eating disorder in DSM-5. Nevertheless, clinicians should be aware that their patients may have its symptoms and specifically inquire about it.



